Abstract
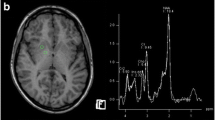
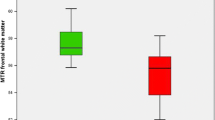
Fifty patients with liver cirrhosis underwent neurological, psychometric, electroencephalographic and biochemical examination as well as cranial magnetic resonance imaging (MRI) to study the incidence of pallidal lesions in cirrhotics and their correlation to liver function, as well as to neurological and mental state. In one patient a histopathological study of the brain was performed. The vast majority of the patients with liver cirrhosis (92%) present with bilateral symmetric pallidal hyperintensities in the T1-weighted MR spin echo sequences, while the T2-weighted images are normal. On the whole there was no correlation between the signal intensity of the pallidal lesions and measures of liver function, neurological status or grade of encephalopathy. As could be shown in follow-up examinations the signal intensity of the lesions increased with decreasing liver function and decreased with normalization of liver function after liver transplantation. The substrate of the lesions remains unclear. However, regions which show alterations in the MRI are histopathologically characterized by the appearance of Alzheimer-type-II cells.
Similar content being viewed by others
References
Adams, R.D., and Foley, J.M. (1953). The neurological disorder associated with liver disease. In Merritt H.H. and Hare C.C (eds)Metabolic and Toxic Diseases of the Nervous System, vn32. Williams and Wilkins, Baltimore, pp. 198–237
Brickenkamp, R. (1981). Test d2. Aufmerksamkeits-Belastungs-Test. Hogrefe J. (ed)Verlag für Psychologie, Göttingen-Toronto-Zürich.
Brunberg, J.A., Kanal, E., Hirsch, W., and Van Thiel, D.H. (1991). Chronic acquired hepatic failure: MR imaging of the brain at 1.5 T.AJNR 12:909–914.
Creutzig, H.O., Schober, Ch., Brölsch, Ch., Pichlmayr, R., and Hundeshagen, H. (1981). The arterial contribution to total liver perfusion.Nucl Med. 20:25–29.
Hamster, W., Kluck, M., and Schomerus, H. (1983). PSE-Syndrom-Test. Kurzform. Duphar Pharma GmbH & Co. KG, Hannover.
Hanner, J.S., Li, K.C.P., and Davis, G.L., (1988). Acquired hepatocerebral degeneration: MR similarity with Wilson Disease.J. Comp. Ass. Tomograph. 12(6): 1076–1077.
Hendrick, R.E. (1988). Image contrast and noise.In Stark D.D. and Bradley W.G. (eds)Magnetic Resonance Imaging. The C.V. Mosby Company, St. Louis, Washington D.C., Toronto; pp. 66–83
Holm, E., Thiele, H., Wolpert, E.M., Reimann-Werle, B. (1980). Neurologische und psychiatrische symptome bei akuten und chronischen Leberkrankheiten.Therapiewoche 30:4790–4806.
Inoue, E., Hori, S., Narumi, Y., Fujita, M., Kuriyama, K., Kadota, T., and Kuroda CH. (1991). Portal-systemic encephalopathy: presence of basal ganglia lesions with high signal intensity on MRI images.Radiology 179:551–555.
Kucharczyk, W., Lenkinski, R.E., Kucharczyk, J., and Henkelman, R.M. (1990). The effect of phospholipid vesicles on the NMR relaxation of water: an explanation for the MR appearance of the neurohypophysis?AJNR 11:693–701.
Kulisevsky, J., Ruscalleda J., Grau J.M. (1991). MR imaging of acquired hepatocerebral degeneration.AJNR 12:527–528.
Kulisevsky, J., Pujol, J., Balanzo, J., Junque, C., Deus, J., Capdevila, A., Villanueva, C. (1992). Pallidal hyperintensity on magnetic resonance imaging in cirrhotic patients: clinical correlations.Hepatology 16:1382–1388.
Kulisevsky, J, Pujol, J., Junque, C., Deus, J., Balanzo, J., and Capdevila, A. (1993). MRI pallidal hyperintensity and brain atrophy in cirrhotic patients: Two different MRI patterns of clinical deterioration?Neurology 43:2570–2573.
Mirowitz, S.A., Westrich, T.J., and Hirsch, J.D. (1991). Hyperintense basal ganglia on T1-weighted MR images in patients receiving parenteral nutrition.Radiology 181:117–120
Moore, J.W., Dunk, A.A., Crawford, J.R., Deans, H., Besson, J.A.O., De Lacy, G.et al. (1989). Neuropsychological deficits and morphological MRI brain scan abnormalities in apparently healthy non-encephalopathic patients with cirrhosis.J. Hepatol. 9:319–325.
Mosher, T.J., Lacey, P.G., Barron, T.F., McNamara, K.P., and Devenyi, A.G. (1994). Increased signal intensity in the basal ganglia on T1-weighted MRI correlates with elevated erythrocyte manganese in patients with chronic liver disease.Proc. Soc. Magnetic Resonance 1:8.
Newland, M.C., Ceckler, T.L., Kordower, J.H., and Weiss, B. (1989). Visualizing manganese in the primate basal ganglia with magnetic resonance imaging.Exp. Neurol. 106:251–258.
Norenberg, M.D. (1977). A light and electron microscopic study of experimental portal-systemic (ammonia) encephalopathy. Progression and reversal of the disorder.Lab. Invest. 36(6):618–626.
Norenberg, M.D. (1987). The role of astrocytes in hepatic encephalopathy.Neurochem. Pathol. 6:13–29.
Parsons-Smith, B.G., Summerskill, W.H.J., Dawson, A.M., and Sherlock, S. (1957). The electroencephalograph in liver disease.Lancet II:867–871
Plum, F., and Hindfelt, B. (1976). The neurological complications of liver disease. In Vinken P.J. and Bruyn G.W. (eds)Handbook of Clinical Neurology Vol. 27. North Holland, Amsterdam, pp. 349–377.
Pomier Layrargues, G., Spahr, L., Butterworth, R.F. (1995). Increased manganese concentrations in pallidum of cirrhotic patients.Lancet 345:735.
Pugh, R.N.H., Murray-Lyon I.M., Dawson, J.L., Pietroni, M.C., and Will, R. (1973). Transection of the oesophagus for bleeding oesophageal varices.Brit. J. Surg. 60(8):646–649.
Pujol, A., Graus, F., Peri, J., Mercader, J.M., and Rimola, A. (1991). Hyperintensity in the globus pallidus on T1-weighted and inversion-recovery MRI: a possible marker of advanced liver disease.Neurology 41(9):1526–1527.
Pujol, A., Pujol, J., Graus, F., Rimola, A., Peri, J., Mercader, J.M.et al. (1993). Hyperintense globus pallidus on T1-weighted MRI in cirrhotic patients is associated with severity of liver failure.Neurology 43:65–69.
Tewes, U. (1991). HAWIE-R. Hamburg-Wechsler Intelligenztest für Erwachsene. Revision 1991. Verlag Hans Huber, Bern-Stuttgart-Toronto.
Uchino, A., Miyoshi, T., and Ohno, M. (1989). Case report - MR imaging of chronic persistent hepatic encephalopathy.Radiat. Med. 7(6):257–260.
Zeneroli, M.L., Cioni, G., Crisi, G., Vezzelli, C., and Ventura, E. (1991). Globus pallidus alterations and brain atrophy in liver cirrhosis patients with encephalopathy: An MR imaging study.Magnet. Res. Imaging 9:295–302. A0431005 00003 CS-SPJRNPDF [HEADSUP]
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Weissenborn, K., Ehrenheim, C., Hori, A. et al. Pallidal lesions in patients with liver cirrhosis: clinical and MRI evaluation. Metab Brain Dis 10, 219–231 (1995). https://doi.org/10.1007/BF02081027
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02081027