Abstract
We studied 42 individuals, including 8 patients with either complete or partial syndrome of mitochondrial myopathy, encephalopathy, lactic acidosis and stroke-like episodes (MELAS), 8 patients with either complete or partial syndrome of myoclonic epilepsy with ragged-red fibers (MERRF) and 26 maternal family members who carried either the A3243G or A8344G mutation of mitochondrial DNA (mtDNA). Clinical manifestations and prognosis were followed up in the patients harboring the A3243G or A8344G mutation. The relationship between clinical features and proportions of mutant mtDNAs in muscle biopsies, blood cells and/or hair follicles was studied. In the 8 regularly followed patients with the A3243G mutation, 4 died within 1 month to 7 years due to status epilepticus and/or recurrent stroke-like episodes. Two patients developed marked mental deterioration and 2 remained stationary. All of the patients harboring the A8344G mutation were stable or deteriorated slightly, except for 1 patient who died due to brain herniation after putaminal hemorrhage. The A3243G and A8344G mtDNA mutations were heteroplasmic in the muscle biopsies, blood cells and hair follicles of both the probands and their maternal family members. The mean proportion of A3243G mutant mtDNA in the muscle biopsies of the patients with MELAS syndrome (68.5 ± 21.3%, range 33–92%) was significantly higher than that of the asymptomatic family members (37.1 ± 12.6%, range 0–51%). The average proportions of A8344G mutant mtDNA in the muscle biopsies (90.1 ± 3.9%, range 89–95%) and hair follicles (93.9 ± 6.4%, range 84–99%) of the patients with MERRF syndrome were also significantly higher than those of the asymptomatic family members (muscle: 40.3 ± 39.5%, range 1–80%; hair follicles: 51.0 ± 44.5%, range 0.1–82%). We concluded that measurement of the proportion of mutant mtDNA in muscle biopsies may provide useful information in the identification of symptomatic patients with mitochondrial encephalomyopathies. For patients with the A3243G mutation, the prognosis was related to status epilepticus and the number of recurrent stroke-like episodes and was much worse than for patients with the A8344G mutation of mtDNA, who had stable or slowly deteriorating clinical courses.
Similar content being viewed by others
References
Chen RS, Huang CC, Chu NS, Chu CC, Shih KD, Pang CY, Wei YH. Tissue distribution of mutant mitochondrial DNA in a patient with MERRF syndrome. Muscle Nerve 94:519–521;1996.
Chen RS, Huang CC, Lee CC, Wai YY, Hsi MS, Pang CY, Wei YH. Overlapping syndrome of MERRF and MELAS: Molecular and neuroradiological studies. Acta Neurol Scand 87:494–498;1993.
Chinnery PF, Howell N, Lightowlers RN, Turnbull DM. Molecular pathology of MELAS and MERRF: The relationship between mutation load and clinical phenotypes. Brain 120:1713–1721;1997.
Chinnery PF, Howell N, Lightowlers RN, Turnbull DM. MELAS and MERRF. The relationship between maternal mutation load and the frequency of clinically affected offspring. Brain 121:1889–1894;1998.
Ciafaloni E, Ricci E, Shanske S, Moraes CT, Silvestri G, Hirano M, Simonetti S, Angelini C, Donati MA, Garcia C. MELAS: Clinical features, biochemistry, and molecular genetics. Ann Neurol 31:391–398;1992.
DiMauro S. Mitochondrial encephalomyopathies. In Rosenberg RN, Prusiner SB, DiMauro S, Barchi RL, Kunkel LM, eds. The Molecular and Genetic Basis of Neurological Disease. Boston, Butterworth-Heinemann, 665–694;1993.
Fang W, Huang CC, Chu NS, Lee CC, Chen RS, Pang CY, Shih KD, Wei YH. Myoclonic epilepsy with ragged-red fibers (MERRF) syndrome: Report of a Chinese family with mitochondrial DNA point mutation in tRNALys gene. Muscle Nerve 17:52–57;1994.
Fang W, Huang CC, Lee CC, Cheng SY, Pang CY, Wei YH. Ophthalmologic manifestations in MELAS syndrome. Arch Neurol 53:977–980;1993.
Goto Y, Horai S, Matsuoka T, Koga Y, Nihei K, Kobayashi M, Nonaka I. Mitochondrial myopathy encephalopathy, lactic acidosis and stroke-like episodes (MELAS): A correlative study of the clinical features and mitochondrial DNA mutation. Neurology 42:545–550;1992.
Goto Y, Nonaka I, Horai S. A mutation in the tRNALeu(UUR) gene associated with the MELAS subgroup of mitochondrial encephalomyopathies. Nature 348:651–653;1990.
Hammans SR, Sweeney MG, Brockington M, Lennox GG, Lawton NF, Kennedy CR, Morgan-Hughes JA, Harding AE. The mitochondrial DNA transfer RNA(Lys)A→G(8344) mutation and the syndrome of myoclonic epilepsy with ragged red fibers (MERRF). Relationship of clinical phenotype to proportion of mutant mitochondrial DNA. Brain 116:617–632;1993.
Hammans SR, Sweeney MG, Hanna MG. The mitochondrial DNA transfer RNALeu (UUR) A3243G mutation. A clinical and genetic study. Brain 118:721–734;1995.
Hasegawa H, Matsuoka T, Goto YI, Nonaka I. Strongly succinate dehydrogenase-reactive blood vessels in muscles from patients with mitochondrial myopathy, encephalopathy, lactic acidosis and stroke-like episodes. Ann Neurol 29:601–605;1991.
Hirano M, Ricci E, Koenigsberger MR, Defendini R, Pavlakis SG, DeVivo DC, DiMauro S, Rowland LP. MELAS: An original case and clinical criteria for diagnosis. Neuromuscul Disord 2:125–135;1992.
Holt IJ, Harding AE, Petty RK, Morgan-Hughes JA. A new mitochondrial disease associated with mitochondrial DNA heteroplasmy. Am J Hum Genet 46:428–433;1990.
Huang CC, Chen RS, Chen CM, Wang HS, Lee CC, Pang CY, Hsu HS, Lee HC, Wei YH. MELAS syndrome with mitochondrial tRNALeu(UUR) gene mutation in a Chinese family. J Neurol Neurosurg Psychiatry 57:586–589;1994.
Huang CC, Chen RS, Chu NS, Pang CY, Wei YH. Random mitotic segregation of mitochondrial DNA in MELAS syndrome. Acta Neurol Scand 93:198–202;1996.
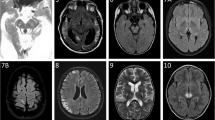
Huang CC, Wai YY, Chu NS, Liou CW, Pang CY, Shih KD, Wei YH. Mitochondrial encephalomyopathies: CT and MRI findings and correlations with clinical features. Eur Neurol 35:199–205; 1995.
Kobayashi Y, Momoi MY, Tominaga K, Momoi T, Nihei K, Yanagisawa M, Kagawa Y, Ohta S. A point mutation in the mitochondrial tRNALeu(UUR) gene in MELAS (mitochondrial myopathy, encephalopathy, lactic acidosis and stroke-like episodes). Biochem Biophys Res Commun 173:816–822;1990.
Koo B, Becker LE, Chuang S, Merante F, Robinson BH, MacGregor D, Tein I, Ho VB, McGreal DA, Wherrett JR. Mitochondrial encephalomyopathy, lactic acidosis and stroke-like episodes (MELAS): Clinical, radiological, pathological, and genetic observations. Ann Neurol 34:25–32;1993.
Larsson NG, Tulinius MH, Holme E, Oldfors A, Andersen O, Wahlstrom J, Aasly J. Segregation and manifestations of the mtDNA tRNA-(Lys) A→G(8344) mutation of myoclonus epilepsy and ragged-red fiber (MERRF) syndrome. Am J Hum Genet 51:1201–1212;1992.
Lee ML, Chaou WT, Yang AD, Jong YJ, Tsai JL, Pang CY, Wei YH. Mitochondrial myopathy, encephalopathy, lactic acidosis and stroke-like episodes (MELAS): Report of a sporadic case and review of the literature. Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi 35:148–156;1994.
Li JY, Kong KW, Chang MH, Cheung SC, Lee HC, Pang CY, Wei YH. MELAS syndrome associated with a tandem duplication in the D-loop of mitochondrial DNA. Acta Neurol Scand 93:450–455;1996.
Liou CW, Huang CC, Chee ECY, Jong YJ, Tsai JL, Pang CY, Lee HC, Wei YH. MELAS syndrome: Correlation between clinical features and molecular genetic analysis. Acta Neurol Scand 90:354–359;1994.
Matsuoka T, Goto Y, Yoneda M, Nonaka I. Muscle histopathology in myoclonus epilepsy with ragged-red fibers (MERRF). J Neurol Sci 106:193–198;1991.
Nonaka I. Mitochondrial diseases. Curr Opin Neurol Neurosurg 5:622–632;1992.
Ozawa M, Goto Y, Sakuta R, Tanno Y, Tsuji S, Nonaka I. The 8344 mutation in mitochondrial DNA: A comparison between the proportion of mutant DNA and clinico-pathologic findings. Neuromuscul Disord 5:483–488;1995.
Pang CY, Huang CC, Yen MY, Wang EK, Kao KP, Chen SS, Wei YH. Molecular epidemiologic study of mitochondrial DNA mutations in patients with mitochondrial diseases in Taiwan. J Formos Med Assoc 98:326–334;1999.
Sakuta R, Nonaka I. Vascular involvement in mitochondrial myopathy. Ann Neurol 25:594–601;1989.
Schon EA, Bonilla E, DiMauro S. Mitochondrial DNA mutations and pathogenesis (review). J Bioenerg Biomembr 29:131–149;1997.
Seibel P, Degoul F, Bonne G, Romero N, Franois D, Paturneau-Jouas M, Zeigler F, Eymard B, Fardeau M, Marsac C, Kadenbach B. Genetic, biochemical and pathophysiological characterization of a family mitochondrial encephalomyopathy (MERRF). J Neurol Sci 105:217–224;1991.
Servidei S. Mitochondrial encephalomyopathies: Gene mutation. Neuromuscul Disord 8:8–9;1998.
Shih KD, Yen TC, Pang CY, Wei YH. Mitochondrial DNA mutation in a Chinese family with myoclonic epilepsy and ragged-red fiber disease (MERRF). Biochem Biophys Res Commun 174:1109–1116;1991.
Shoffner JM, Lott MT, Lezza AM, Seibel P, Ballinger SW, Wallace DC. Myoclonic epilepsy and ragged-red fiber disease (MERRF) is associated with a mitochondrial DNA tRNALys mutation. Cell 61:931–937;1990.
Silvestri G, Ciafaloni E, Santorelli FM, Shanske S, Servidei S, Graf WD, Sumi M, DiMauro S. Clinical features associated with the A→G transition at nucleotide 8344 of mtDNA (MERRF mutation). Neurology 43:1200–1206;1993.
Tanno Y, Yoneda M, Nonaka I, Tanaka K, Miyatake T, Tsuji S. Quantitation of mitochondrial DNA carrying tRNALys mutation in MERRF patients. Biochem Biophys Res Commun 179:880–885;1991.
Vilarinho L, Sanforelli FM, Coelho I, Rodrigues L, Maia M, Barafa I, Cabral P, Dionisio A, Costa A, Guimaraes A, DiMauro S. The mitochondrial DNA A3243G mutation in Portugal: Clinical and molecular studies in 5 families. J Neurol Sci 163:168–174;1999.
Yang CC, Hwang CC, Pang CY, Wei YH. Mitochondrial myopathy with predominant respiratory dysfunction in a patient with A3243G mutation in the mitochondrial tRNALeu(UUR) gene. J Formos Med Assoc 91:715–719;1998.
Yang CY, Lam HC, Lee HC, Wei YH, Lu CC, Han TM, Tsai JL, Chuang YH, Lee JK. MELAS syndrome associated with diabetes mellitus and hyperthyroidism: A case report from Taiwan. Clin Endocrinol (Oxf) 43:235–239;1995.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Huang, CC., Kuo, HC., Chu, CC. et al. Clinical phenotype, prognosis and mitochondrial DNA mutation load in mitochondrial encephalomyopathies. J Biomed Sci 9, 527–533 (2002). https://doi.org/10.1007/BF02254979
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02254979