Abstract
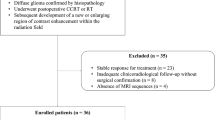
Advanced magnetic resonance (MR) imaging techniques provide physiologic information that complements the anatomic information available from conventional MR imaging. We evaluated the roles of diffusion and perfusion imaging for the assessment of grade and type of histologically proven intraaxial brain tumors. A total of 28 patients with intraaxial brain tumors underwent conventional MR imaging (T2- and T1-weighted sequences after gadobenate dimeglumine injection), diffusion imaging and T2*-weighted echo-planar perfusion imaging. Examinations were performed on 19 patients during initial diagnosis and on nine patients during follow-up therapy. Determinations of relative cerebral blood volume (rCBV) and apparent diffusion coefficient (ADC) were performed in the solid parts of each tumor, peritumoral region and contralateral white matter. For gliomas, rCBV values were greater in high-grade than in low-grade tumors (3.87±1.94 versus 1.30±0.42) at the time of initial diagnosis. rCBV values were increased in all recurrent tumors, except in one patient who presented with a combination of recurrent glioblastoma and massive radionecrosis on histology. Low-grade gliomas had low rCBV even in the presence of contrast medium enhancement. Differentiation between high- and low-grade gliomas was not possible using diffusion-weighted images and ADC values alone. In the peritumoral areas of untreated high-grade gliomas and metastases, the mean rCBV values were higher for high-grade gliomas (1.7±0.37) than for metastases (0.54±0.18) while the mean ADC values were higher for metastases. The rCBV values of four lymphomas were low and the signal intensity–time curves revealed a significant increase in signal intensity after the first pass of gadobenate dimeglumine. Diffusion and perfusion imaging, even with relatively short imaging and data processing times, provide important information for lesion characterization.





Similar content being viewed by others
References
Cha S, Knopp EA, Johnson G, Wetzel SG, Litt AW, Zagzag D (2002) Intracranial mass lesions: dynamic contrast-enhanced susceptibility-weighted echo-planar perfusion MR imaging. Radiology 223:11–29
Yang D, Korogi Y, Sugahara T, et al (2002) Cerebral gliomas: prospective comparison of multivoxel 2D chemical-shift imaging proton MR spectroscopy, echoplanar perfusion and diffusion-weighted MRI. Neuroradiology 44:656–666
Harting I, Hartmann M, Bonsanto MM, et al (2004) Characterization of necrotic meningioma using diffusion MRI, perfusion MRI, and MR spectroscopy: case report and review of the literature. Neuroradiology 46:189–193
Daumas-Duport C, Beuvon F, Varlet P, Fallet-Bianco C (2000) Gliomas: WHO and Sainte-Anne Hospital classifications. Ann Pathol 20:413–428
Law M, Yang S, Wang H, et al (2003) Glioma grading: sensitivity, specificity, and predictive values of perfusion MR imaging and proton MR spectroscopic imaging compared with conventional MR imaging. AJNR Am J Neuroradiology 24:1989–1998
Knopp EA, Cha S, Johnson G, et al (1999) Glial neoplasms: dynamic contrast-enhanced T2*-weighted MR imaging. Radiology 211:791–798
Knopp MV, Runge VM, Essig M, et al (2004) Primary and secondary brain tumors at MR imaging: bicentric intraindividual crossover comparison of gadobenate dimeglumine and gadopentetate dimeglumine. Radiology 230:55–64
Colosimo C, Knopp MV, Barreau X, et al (2004) A comparison of Gd-BOPTA and Gd-DOTA for contrast-enhanced MRI of intracranial tumours. Neuroradiology 46:655–665
Brem S, Cotran R, Folkman J (1972) Tumor angiogenesis: a quantitative method for histologic grading. J Natl Cancer Inst 48:347–356
Shin JH, Lee HK, Kwun BD, et al (2002) Using relative cerebral blood flow and volume to evaluate the histopathologic grade of cerebral gliomas: preliminary results. AJR Am J Roentgenol 179:783–789
Provenzale JM, Wang GR, Brenner T, Petrella JR, Sorensen AG (2002) Comparison of permeability in high-grade and low-grade brain tumors using dynamic susceptibility contrast MR imaging. AJR Am J Roentgenol 178:711–716
Law M, Yang S, Babb JS, et al (2004) Comparison of cerebral blood volume and vascular permeability from dynamic susceptibility contrast-enhanced perfusion MR imaging with glioma grade. AJNR Am J Neuroradiol 25:746–755
Weber MA, Risse F, Giesel FL, Schad LR, Kauczor HU, Essig M (2005) Perfusion measurement using the T2* contrast media dynamics in neuro-oncology. Physical basics and clinical applications. Radiologe 45:618–632
Aronen HJ, Gazit IE, Louis DN, et al (1994) Cerebral blood volume maps of gliomas: comparison with tumor grade and histologic findings. Radiology 191:41–51
Sugahara T, Korogi Y, Kochi M, et al (1998) Correlation of MR imaging-determined cerebral blood volume maps with histologic and angiographic determination of vascularity of gliomas. AJR Am J Roentgenol 171:1479–1486
Lam WW, Poon WS, Metreweli C (2002) Diffusion MR imaging in glioma: does it have any role in the pre-operation determination of grading of glioma? Clin Radiol 57:219–225
Coulon A, Lafitte F, Hoang-Xuan K, et al (2002) Radiographic findings in 37 cases of primary CNS lymphoma in immunocompetent patients. Eur Radiol 12:329–340
Hartmann M, Heiland S, Harting I, et al (2003) Distinguishing of primary cerebral lymphoma from high-grade glioma with perfusion-weighted magnetic resonance imaging. Neurosci Lett 338:119–122
Guo AC, Cummings TJ, Dash RC, Provenzale JM (2002) Lymphomas and high-grade astrocytomas: comparison of water diffusibility and histologic characteristics. Radiology 224:177–183
Chiang IC, Kuo YT, Lu CY, et al (2004) Distinction between high-grade gliomas and solitary metastases using peritumoral 3-T magnetic resonance spectroscopy, diffusion, and perfusion imagings. Neuroradiology 46:619–627
Krabbe K, Gideon P, Wagn P, Hansen U, Thomsen C, Madsen F (1977) MR diffusion imaging of human intracranial tumours. Neuroradiology 39:483–489
Sugahara T, Korogi Y, Tomiguchi S, et al (2000) Posttherapeutic intraaxial brain tumor: the value of perfusion-sensitive contrast-enhanced MR imaging for differentiating tumor recurrence from nonneoplastic contrast-enhancing tissue. AJNR Am J Neuroradiol 21:901
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rollin, N., Guyotat, J., Streichenberger, N. et al. Clinical relevance of diffusion and perfusion magnetic resonance imaging in assessing intra-axial brain tumors. Neuroradiology 48, 150–159 (2006). https://doi.org/10.1007/s00234-005-0030-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-005-0030-7