Abstract
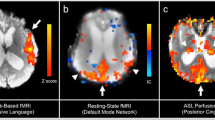
Background: Traumatic brain injury is a major cause of disability and death in the pediatric population. The metabolic and neurochemical abnormalities that underlie traumatic brain injury remain poorly understood, but hypoxia-ischemic injury might play an important role. Objective: This study evaluated children with inflicted traumatic brain injury using magnetic resonance spectroscopy (MRS). We postulated that children with hypoxic-ischemic injury indicated by elevated lactate in the acute phase of injury will have worse early neurological status and short-term clinical outcomes than those without lactate upon MRS. Materials and methods: This prospective study employed proton MRS to sample bilaterally the frontal lobes and the parasagittal cortex within the parietal and occipital lobes of 11 patients with inflicted traumatic brain injury who were undergoing a clinical MRI examination. Patients’ measured clinical course while hospitalized included initial neurological evaluation, presence of seizure activity, need for admission to the pediatric intensive care unit (PICU), number of days hospitalized, presence of retinal hemorrhages and presence of bone fractures. Measurement of outcome was determined using the Pediatric Overall Performance Category Scale (POPCS; 1 = good performance; 6 = death). Results: Four children demonstrated elevated lactate and diminished N-acetyl aspartate (a neuronal marker) within several regions, indicating global ischemic injury (lactate-positive global group). These four children all had seizure activity and abnormal initial neurological examinations and required admission to the PICU. The mean POPCS for this group was 3.25. In four other children, lactate was detected within at least one region, indicating a focal ischemic injury (lactate-positive focal group); two of these children had seizure activity, and two had an abnormal initial neurological examination. The mean POPCS score was 1.5 for this group. The remaining three children had no evidence of lactate upon MRS (lactate-negative group). These children did not have seizure activity, did not require admission to the PICU, nor did they have initial abnormal neurological examinations. The mean POPCS score was 1.3 for this group. Summary: Patients with inflicted traumatic brain injury and evidence of hypoxic-ischemic injury as indicated by elevated lactate on MRS tend to have worse early neurological status and early outcome scores. Lactate levels as sampled by MRS might predict early clinical outcome in inflicted traumatic brain injury.



Similar content being viewed by others
References
Lescohier I, DiScala C, Caffey J (1993) Blunt trauma in children: causes and outcomes of head versus extracranial injury. Pediatrics 91:721–725
Caffey J (1972) On the theory and practice of shaking infants: its potential residual effects of permanent brain damage and mental retardation. Am J Dis Child 124:161–169
Ewing-Cobbs L, Kramer L, Prasad M (1998) Neuroimaging, physical and developmental findings after inflicted and noninflicted traumatic brain injury in young children. Pediatrics 102:300–307
Makoroff KL, Putnam FW (2003) Outcomes in inflicted traumatic brain injury. Dev Med Child Neurol 45:497–502
Johnson DL, Boal D, Baule R (1995) Role of apnea in nonaccidental head injury. Pediatr Neurosurg 23:305–310
Barlow KM, Minns RA (1999) The relationship between intracranial pressure and outcome in non-accidental head injury. Dev Med Child Neurol 4:220–225
Cecil KM, Jones BV (2001) Magnetic resonance spectroscopy of the pediatric brain. Top Magn Reson Imag 12:435–452
Lanfermann H, Kugel H, Heindel W, et al (1995) Metabolic changes in acute and subacute cerebral infarctions: findings at proton MR spectroscopic imaging. Radiology 196:203–210
Fiser DH (1992) Assessing the outcome of pediatric intensive care. J Pediatr 121:68–74
Webb PG, Sailasuta N, Kohler SJ, et al (1994) Automated single-voxel proton MRS: technical development and multisite verification. Magn Reson Med 31:365–373
Marquardt DW (1963) An algorithm for least-squares estimation on nonlinear parameters. J Soc Ind Appl Math 11:431–441
Haseler LJ, Phil M, Arcinue E, et al (1997) Evidence from proton magnetic resonance spectroscopy for a metabolic cascade of neuronal damage in shaken baby syndrome. Pediatrics 99:4–14
Holshouser BA, Ashwal S, Luh GY, et al (1997) Proton MR spectroscopy after acute central nervous system injury: outcome prediction in neonates, infants, and children. Radiology 202:487–496
Ashwal S, Holshouser BA, Shu SK, et al (2000) Predictive value of proton magnetic resonance spectroscopy in pediatric closed-head injury. Pediatr Neurol 23:114–125
Kadri M, Shu S, Holhouser B, et al (2003) Proton magnetic resonance spectroscopy improves outcome prediction in perinatal CNS insults. J Perinatol 23:181–185
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Makoroff, K.L., Cecil, K.M., Care, M. et al. Elevated lactate as an early marker of brain injury in inflicted traumatic brain injury. Pediatr Radiol 35, 668–676 (2005). https://doi.org/10.1007/s00247-005-1441-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-005-1441-7