Abstract
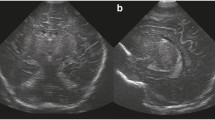
Patterns of damage in the mature neonatal brain can be subdivided into focal, multifocal and diffuse. The main cause of diffuse brain damage in the term newborn is hypoxic–ischaemic encephalopathy (HIE). HIE is still the major recognized perinatal cause of neurological morbidity in full-term newborns. MRI offers today the highest sensitivity in detecting acute anoxic injury of the neonatal brain. Conventional acquisition techniques together with modern diffusion techniques can identify typical patterns of HIE injury, even in the early course of the disease. However, even though highly suggestive, these patterns cannot be considered as pathognomonic. Perinatal metabolic disease such as kernicterus and severe hypoglycaemia should be differentiated from classic HIE. Other conditions, such as infections, non-accidental injury and rarer metabolic diseases can be misinterpreted as HIE in their early course when diffuse brain swelling is still the predominant MRI feature. Diffusion techniques can help to differentiate different types of diffuse brain oedema. Typical examples of focal injuries are arterial or venous infarctions. In arterial infarction, diffusion techniques can define more precisely than conventional imaging the extent of focal infarction, even in the hyperacute phase. Moreover, diffusion techniques provide quantitative data of acute corticospinal tract injury, especially at the level of the cerebral peduncles. Venous infarction should be suspected in every case of unexplained cerebral haematoma in the full-term newborn. In the presence of spontaneous bleeding, venous structures should always be evaluated by MR angiography.













Similar content being viewed by others
References
Volpe JJ (2001) Neurology of the newborn, 4th edn. Saunders, Philadelphia
Chugani HT, Phelps ME, Mazziotta JC (1987) Positron emission tomography study of human brain functional development. Ann Neurol 22:487–497
Barkovich AJ (2005) Pediatric neuroimaging, 4th edn. Lippincott, Williams & Wilkins, Philadelphia
Triulzi F, Baldoli C, Parazzini C (2001) Neonatal MR imaging. Magn Reson Imaging Clin N Am 9:57–82
Robertson RL, Ben-Sira L, Barnes PD, et al (1999) MR line-scan diffusion-weighted imaging of term neonates with perinatal brain ischemia. AJNR 20:1658–1670
Barkovich AJ, Westmark KD, Bedi HS, et al (2001) Proton spectroscopy and diffusion imaging on the first day of life after perinatal asphyxia: preliminary report. AJNR 22:1786–1794
McKinstry RC, Miller JH, Snyder AZ, et al (2002) A prospective, longitudinal diffusion tensor imaging study of brain injury in newborns. Neurology 59:824–833
Rutherford M, Counsell S, Allsop J, et al (2004) Diffusion-weighted magnetic resonance imaging in term perinatal brain injury: a comparison with site of lesion and time from birth. Pediatrics 114:1004–1014
Hunt RW, Neil JJ, Coleman LT, et al (2004) Apparent diffusion coefficient in the posterior limb of the internal capsule predicts outcome after perinatal asphyxia. Pediatrics 114:999–1003
Groenendaal F, Veenhoven RH, van der Grond J, et al (1994) Cerebral lactate and N-acetyl-aspartate/choline ratios in asphyxiated full-term neonates demonstrated in vivo using proton magnetic resonance spectroscopy. Pediatr Res 35:148–151
Zarifi MK, Astrakas LG, Poussaint TY, et al (2002) Prediction of adverse outcome with cerebral lactate level and apparent diffusion coefficient in infants with perinatal asphyxia. Radiology 225:859–870
Cappellini M, Rapisardi G, Cioni ML, et al (2002) Acute hypoxic encephalopathy in the full-term newborn: correlation between magnetic resonance spectroscopy and neurological evaluation at short and long term. Radiol Med 104:332–340
Martich-Kriss V, Kollias SS, Ball WS Jr (1995) MR findings in kernicterus. AJNR 16:819–821
Govaert P, Lequin M, Swarte R, et al (2003) Changes in globus pallidus with (pre)term kernicterus. Pediatrics 112:1256–1263
Barkovich AJ, Ali FA, Rowley HA, et al (1998) Imaging patterns of neonatal hypoglycaemia. AJNR 19:592–593
Takanashi J, Barkovich AJ, Cheng SF, et al (2003) Brain MR imaging in neonatal hyperammonemic encephalopathy resulting from proximal urea cycle disorders. AJNR 24:1184–1187
Khong PL, Lam BC, Chung BH, et al (2003) Diffusion-weighted MR imaging in neonatal nonketotic hyperglycinemia. AJNR 24:1181–1183
Teixeira J, Zimmerman RA, Haselgrove JC, et al (2001) Diffusion imaging in pediatric central nervous system infections. Neuroradiology 43:1031–1039
Kurtz J, Anslow P (2003) Infantile herpes simplex encephalitis: diagnostic features and differentiation from non-accidental injury. J Infect 46:12–16
Righini A, Ramenghi L, Zirpoli S, et al (2005) Brain apparent diffusion coefficient decrease during correction of severe hypernatremic dehydration. AJNR 26:1690–1694
Righini A, Ramenghi LA, Parini R, et al (2003) Water apparent diffusion coefficient and T2 changes in the acute stage of maple syrup urine disease: evidence of intramyelinic and vasogenic-interstitial edema. J Neuroimaging 13:162–165
Lynch JK, Hirtz DG, De Veber G, et al (2002) Report of National Institute of Neurological Disorders and Stroke workshop on perinatal and childhood stroke. Pediatrics 109:116–123
Krishnamoorthy K, Soman T, Takeoka M, et al (2000) Diffusion-weighted imaging in neonatal cerebral infarction: clinical utility and follow-up. J Child Neurol 15:592–602
De Vries LS, Van der Gron J, Van Haastert IC, et al (2005) Prediction of outcome in new-born infants with arterial ischemic stroke using diffusion-weighted magnetic resonance imaging. Neuropediatrics 36:12–20
Carvalho KS, Bodensteiner JB, Connolly PJ, et al (2001) Cerebral venous thrombosis in children. J Child Neurol 16:574–580
Acknowledgements
We wish to thank the NICU, and the Pediatric Neurology of Children’s Hospital, “V. Buzzi”, and the NICU-Ospedale Maggiore, CI Mangiagalli-IRCCS-University of Milan for the continuous cooperation and support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Triulzi, F., Parazzini, C. & Righini, A. Patterns of damage in the mature neonatal brain. Pediatr Radiol 36, 608–620 (2006). https://doi.org/10.1007/s00247-006-0203-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-006-0203-5