Abstract
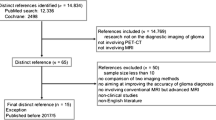
These joint practice guidelines, or procedure standards, were developed collaboratively by the European Association of Nuclear Medicine (EANM), the Society of Nuclear Medicine and Molecular Imaging (SNMMI), the European Association of Neurooncology (EANO), and the working group for Response Assessment in Neurooncology with PET (PET-RANO). Brain PET imaging is being increasingly used to supplement MRI in the clinical management of glioma. The aim of these standards/guidelines is to assist nuclear medicine practitioners in recommending, performing, interpreting and reporting the results of brain PET imaging in patients with glioma to achieve a high-quality imaging standard for PET using FDG and the radiolabelled amino acids MET, FET and FDOPA. This will help promote the appropriate use of PET imaging and contribute to evidence-based medicine that may improve the diagnostic impact of this technique in neurooncological practice. The present document replaces a former version of the guidelines published in 2006 (Vander Borght et al. Eur J Nucl Med Mol Imaging. 33:1374–80, 2006), and supplements a recent evidence-based recommendation by the PET-RANO working group and EANO on the clinical use of PET imaging in patients with glioma (Albert et al. Neuro Oncol. 18:1199–208, 2016). The information provided should be taken in the context of local conditions and regulations.
Similar content being viewed by others
Preamble
The Society of Nuclear Medicine and Molecular Imaging (SNMMI) is an international scientific and professional organization founded in 1954 to promote the science, technology, and practical application of nuclear medicine. Its 18,000 members are physicians, technologists and scientists specializing in the research and practice of nuclear medicine. In addition to publishing journals, newsletters and books, the SNMMI also sponsors international meetings and workshops designed to increase the competencies of nuclear medicine practitioners and to promote new advances in the science of nuclear medicine. The European Association of Nuclear Medicine (EANM) is a professional nonprofit medical association that facilitates communication worldwide among individuals pursuing clinical and research excellence in nuclear medicine, and had 2,800 members in 2017. The EANM was founded in 1985.
The SNMMI/EANM will periodically define new standards/guidelines for nuclear medicine practice to help advance the science of nuclear medicine and to improve the quality of service to patients. Existing standards/guidelines will be reviewed for revision or renewal, as appropriate, on their fifth anniversary or sooner, if indicated. As of February 2014, the SNMMI guidelines will now be referred to as procedure standards. Any previous practice guidelines or procedure guidelines that describe how to perform a procedure are now considered SNMMI procedure standards. Each of the standards/guidelines, that represents a policy statement by the SNMMI/EANM, has undergone a thorough consensus process in which it has been subjected to extensive review. The SNMMI/EANM recognizes that the safe and effective use of diagnostic nuclear medicine imaging requires specific training, skills and techniques, as described in each document.
The EANM and SNMMI have written and approved these standards/guidelines to promote the use of nuclear medicine procedures of high quality. These standards/guidelines are intended to assist practitioners in providing appropriate nuclear medicine care for patients. They are not inflexible rules or requirements of practice and are not intended, nor should they be used, to establish a legal standard of care. For these reasons and those set forth below, the SNMMI/EANM cautions against the use of these standards/guidelines in litigation in which the clinical decisions of a practitioner are called into question.
The ultimate judgment regarding the propriety of any specific procedure or course of action must be made by medical professionals taking into account the unique circumstances of each case. Thus, there is no implication that an approach differing from the standards/guidelines, standing alone, is below the standard of care. To the contrary, a conscientious practitioner may responsibly adopt a course of action different from that set forth in the standards/guidelines when, in the reasonable judgment of the practitioner, such course of action is indicated by the condition of the patient, limitations of available resources, or advances in knowledge or technology subsequent to publication of the standards/guidelines.
The practice of medicine involves not only the science but also the art of dealing with the prevention, diagnosis, alleviation and treatment of disease. The variety and complexity of human conditions make it impossible to always reach the most appropriate diagnosis or to predict with certainty a particular response to treatment. Therefore, it should be recognized that adherence to these standards/guidelines will not ensure an accurate diagnosis or a successful outcome. All that should be expected is that the practitioner will follow a reasonable course of action based on current knowledge, available resources and the needs of the patient to deliver effective and safe medical care. The sole purpose of these standards/guidelines is to assist practitioners in achieving this objective.
The present guidelines/standards were developed collaboratively by the EANM and SNMMI with the European Association of Neurooncology (EANO) and the working group for Response Assessment in Neurooncology with PET (PET-RANO). They summarize the views of the Neuroimaging, Oncology and Physics Committees of the EANM, the Brain Imaging Council of the SNMMI, the EANO, and PET-RANO, and reflect recommendations for which the EANM cannot be held responsible. The recommendations should be taken into the context of good practice of nuclear medicine and do not substitute for national and international legal or regulatory provisions.
Introduction
Gliomas are the second most common primary brain tumour with an annual incidence rate of around six cases per 100,000 individuals worldwide [1]. Gliomas represent approximately 27% of all central nervous system (CNS) tumours and 80% of malignant CNS tumours, and are a leading cause of cancer mortality in adults. The most common of all malignant brain and CNS tumours is glioblastoma (46%) which is associated with a median overall survival of 15 months in patients treated with maximal safe tumour resection, concomitant radiotherapy/chemotherapy and adjuvant chemotherapy [2].
Magnetic resonance imaging (MRI) is the primary clinical imaging modality in patients with glioma at all disease stages including the primary evaluation, presurgical planning, early postsurgical evaluation of residual tumour, radiotherapy planning, surveillance during chemotherapy, and definition of recurrence.
There are defined objective and standardized MRI-based criteria for response assessment in neurooncology (RANO) applied to clinical trials in patients with brain tumours. However, MRI contrast enhancement can be unreliable as a surrogate for tumour size or growth. It nonspecifically reflects vascular surface area and the permeability of the contrast agent across a disrupted blood–tumour barrier and may represent tumour biology or a number of other factors including therapy-induced inflammation. Contrast enhancement can be influenced by therapeutics that affect tumour vascular permeability, such as corticosteroid, antiangiogenic [3] or immunotherapy agents [4]. Because of the growing awareness of significant limitations of MRI in the management of glioma, the RANO criteria were recently updated [5]. Hence, to identify infiltrative glioma tissue, the RANO definition of tumour progression was supplemented by inclusion of “significant” enlarging areas of nonenhancing tumour on MRI T2-weighted and fluid-attenuated inversion recovery (FLAIR) image sequences. However, precise quantification of increases in the T2/FLAIR signal could not be defined and other causes of increased T2 or FLAIR signal, such as radiation effects, demyelination, ischaemic injury and oedema have to be considered in the evaluation of progression.
Molecular imaging using positron emission tomography (PET) is a well-established method in systemic oncology [6], and is being increasingly used to supplement MRI in the clinical management of glioma [7,8,9]. PET imaging could have an important role in clinical trials of new strategies for the treatment of glioma, e.g. immunotherapy, where pseudoprogression is particularly challenging for MRI [4]. Recently an evidence-based recommendation by the PET-RANO working group and EANO on the clinical use of PET imaging in gliomas has been published focusing on radiotracers used in clinical practice imaging, i.e. glucose metabolism, 2-deoxy-2-[18F]fluoro-D-glucose (FDG), and system L amino acid transport comprising [11C-methyl]-methionine (MET), O-(2-[18F]fluoroethyl)-L-tyrosine (FET) and 3,4-dihydroxy-6-[18F]fluoro-L-phenylalanine (FDOPA) [7].
The present guidelines/standards focus on the technical aspects of PET image acquisition with the above-mentioned radiotracers, and thus replace all previously published guidelines on glioma imaging [10].
Aim
The aim of these standards/guidelines is to assist nuclear medicine practitioners in recommending, performing, interpreting, and reporting the results of brain PET imaging in patients with glioma.
Definitions
-
1.
PET systems provide static, dynamic or gated images of the distribution of positron-emitting radionuclides within the body by detecting pairs of photons produced in coincidence by the annihilation of a positron and an electron. PET images are produced by a reconstruction process using the coincidence pair data.
-
2.
PET is generally combined with computed tomography (CT) in a single system (PET/CT). Combined PET/MRI systems are also available for clinical use but are currently less widely available.
-
3.
Nuclear medicine computer systems and software applications collect, quantitate, analyse and display the imaging information.
Common clinical indications
Common indications for PET imaging in glioma include, but are not limited to, the following [7]:
-
1.
At primary diagnosis
-
(a)
Differentiation of grade III and IV tumours from nonneoplastic lesions or grade I and II gliomas
-
(b)
Prognostication of gliomas
-
(c)
Definition of the optimal biopsy site (e.g. site of maximum tracer uptake)
-
(d)
Delineation of tumour extent for surgery and radiotherapy planning
-
(a)
-
2.
Diagnosis of tumour recurrence
-
(a)
Differentiation of glioma recurrence from treatment-induced changes, e.g. pseudoprogression, radionecrosis
-
(a)
-
3.
Disease and therapy monitoring
-
(a)
Detection of malignant transformation in grade I and II gliomas
-
(b)
Response assessment during and after radiotherapy and/or chemotherapy
-
(c)
Differentiation of tumour response from pseudoresponse during antiangiogenic therapy
-
(a)
The performances of the PET tracers presented in this guideline are different as discussed in a recent evidence-based recommendation [7].
FDG PET plays a more limited role than amino acid PET in the imaging of gliomas due to the high physiological uptake of FDG in normal brain grey matter and variable uptake by inflammatory lesions. FDG PET is most often used to distinguish tumour recurrence from radiation necrosis in enhancing brain lesions or to distinguish glioma from CNS lymphoma or opportunistic infection.
Qualifications and responsibilities of personnel
Physician
PET examinations should be performed by, or under the supervision of, a physician specialized in nuclear medicine and certified by accreditation boards. In Europe, the certified nuclear medicine physician who performed the study and signed the report is responsible for the procedure, according to national laws and rules. In the United States, the SNMMI Procedure Guideline for General Imaging (Society of Nuclear Medicine, 2010. http://snmmi.files.cms-plus.com/docs/General_Imaging_Version_6.0.pdf) should be consulted.
Technologist
PET examinations should be performed by a qualified registered/certified nuclear medicine technologist. The following documents should be consulted: Performance Responsibility and Guidelines for Nuclear Medicine Technologists 3.1 and the EANM Benchmark Document Nuclear Medicine Technologists’ Competencies (http://www.eanm.org/content-eanm/uploads/2016/11/EANM_2017_TC_Benchmark.pdf [11]). In some jurisdictions, additional qualifications may be necessary for technologists to operate the CT or MR components.
Physicist
PET examinations should be performed using PET systems that comply with national or international quality standards (see section Quality control and improvement). A certified clinical physicist is responsible for ensuring that PET systems meet these quality standards. Moreover, in some countries it is required that a board-certified medical physicist be available to advise the above-mentioned personnel in running the imaging systems and/or in managing dysfunction or failure of the systems, and to perform the examinations. In addition, examinations should be performed following national or international dosimetry and radiation safety standards in relation to both patients and personnel.
Examination procedures/specifications
Recommendations for FDG-specific procedures are defined in previous guidelines, and only recommendations that are new or particular to glioma are discussed [12, 13].
Request
A nuclear medicine imaging facility staff member should check with the nuclear pharmacy provider as to the availability of the radiotracer before scheduling the examination. Advanced notice may be required for tracer delivery.
The study requisition should include:
-
1.
Appropriate clinical information about the patient and a clearly specified clinical question to justify the study and to allow appropriate examination/study coding (see section Common clinical indications).
-
2.
Information about the ability of the patient to cooperate with the examination and the participation of a carer may be helpful.
-
3.
Information about current medications, including glucocorticoids, for correct study interpretation and to avoid unwanted pharmacological interaction effects if mild sedation is necessary.
-
4.
History of prior therapy, including prior chemotherapy, surgery and radiotherapy, which might affect radiopharmaceutical distribution.
-
5.
Results of pertinent imaging studies, resections and biopsies performed, and laboratory results.
-
6.
For PET/MRI, all patients should be screened at request for relevant contraindications to MRI using a standardized checklist (e.g. pregnancy, contrast agent reactions, implants, ports, catheters, metallic implants, vascular stents, coils, active implants, cardiac pacemakers, claustrophobia, etc.) [14].
Patient preparation and precautions
-
1.
The height and body weight of the patient must be documented for measurement of standardized uptake values (SUV; see section Static FET, MET, FDOPA PET, item 1).
-
2.
Recent morphological imaging with MRI (T1, T1 + contrast medium, T2/FLAIR) should be available for image fusion.
-
3.
The patient should be informed about the procedure to guarantee optimal compliance.
-
4.
The patient should be able to lie down quietly for at least 30 to 40 min.
-
5.
If sedation is required for MET, FET or FDOPA imaging, it should start about 20–60 min before the examination. If sedation is required for FDG imaging, sedation should start as late as possible after FDG administration, ideally at least 30 min after FDG injection but prior to imaging.
-
6.
The patient should be required to fast before the examination to ensure stable metabolic conditions. A minimum 4-h fast is recommended for MET, FET, FDOPA, and FDG imaging.
-
7.
Serum glucose should/may be measured before FDG administration so that the interpreting physician is aware of the potential for altered biodistribution.
-
8.
Before scanning, patients should empty their bladder for maximum comfort during the study and in order to reduce the absorbed dose to the bladder (see section Radiation safety).
-
9.
In pregnant patients, it is necessary to make a clinical decision that weighs the benefits to the patient against possible harm [6].
-
10.
For FDOPA PET, premedication with carbidopa is not necessary. Most published studies to date with FDOPA PET in patients with brain tumour have not used carbidopa or other inhibitors of peripheral FDOPA metabolism.
-
11.
If the PET study is to be acquired as part of a PET/MRI study:
-
(a)
Check MRI contraindications from checklist (see section Request, item 6).
-
(b)
Remove all metal from the patient (e.g. dental prostheses, clothing with zippers and buttons), and provide cotton clothing for the patient.
-
(c)
In patients with an implant, the specific type of implant, its location and its component materials need to be known before an MRI examination. The patient should be asked for an implant pass. The safety level of an implant/device should be checked with the manufacturer (e.g. online): “MRI unsafe” is an absolute contraindication; “MRI conditional” is a relative contraindication, conditions apply; “MRI safe” is no contraindication.
-
(d)
If the patient has a metal implant or active device labelled “MRI conditional”, information should be obtained about all the conditions that may apply for safe MRI examination (e.g. from the implant pass or online).
-
(e)
Beyond safety concerns, implants may cause artefacts, large-volume signal voids and geometric distortions on MRI images. These may hamper image reading.
-
(a)
-
12.
It is recommended that the patient stay well hydrated and empty the bladder often.
Radiopharmaceuticals
-
2-Deoxy-2-[18F]fluoro-D-glucose; fludeoxyglucose F18 (FDG)
-
O-(2-[18F]Fluoroethyl)-L-tyrosine (FET)
-
L-[methyl-11C]Methionine; methionine C11 (MET)
-
3,4-Dihydroxy-6-[18F]fluoro-L-phenylalanine; fluorodopa F18 (FDOPA)
Preparation of radiopharmaceuticals
All radiopharmaceuticals must be prepared by qualified personnel according to cGMP-compliant methods that conform to regulatory requirements. The radiopharmaceutical is delivered ready to use. Quality control (QC) is carried out by the manufacturer prior to delivery of the final product.
Administered activity in adults
The recommended injected activities for brain imaging in adults are as follows:
-
18F-FET: 185–200 MBq
-
11C-MET: 370–555 MBq
-
18F-FDOPA: 185–200 MBq
-
18F-FDG: 185–200 MBq
Administered activity in children
In children, the radioactivity dose should be calculated as a fraction of the dose for adults according to the child’s body weight using the factors provided by the EANM Paediatric Task Group [15]. The administered dose may be reduced in systems with higher sensitivity (see section Radiation safety).
The above radiopharmaceuticals should be injected as a bolus.
PET acquisition protocols
Positioning
The scan should be performed with the patient positioned with the head in a dedicated holder and the arms along the body. The entire brain should be in the field of view, including the entire cerebellum, and extreme neck extension or flexion should be avoided.
Head stability
-
1.
The patient should be instructed immediately before the PET acquisition to avoid head movements during all parts of the investigation.
-
2.
Head stability can be achieved by positioning the patient comfortably with the head secured as completely as possible in the dedicated holder. Tape, padding or other flexible head restraints including a thermoplastic mould and vacuum mattress for children may be employed and are often helpful particularly for radiotherapy planning.
-
3.
During the entire investigation, the patient should be continuously visually monitored. Monitoring is particularly important in patients with tumour-associated seizures. Seizure activity during the uptake phase of FDG and FET can lead to increased uptake in the brain affected by seizure activity and can be mistaken for tumour.
PET imaging sequence
The preferred PET imaging sequence is:
-
1.
CT scout topogram for PET/CT to set up the field of view.
-
2.
For attenuation correction (see section Attenuation correction below), a low-dose CT scan, MRI attenuation correction scan or transmission scan should be performed. Mathematical attenuation correction (i.e. based on the patient’s external contour (derived from a PET image without attenuation correction) should not be applied.
-
3.
Static or dynamic single field of view PET acquisition.
Attenuation correction
Images should be acquired in 3D data acquisition mode and attenuation correction should be based on a low-dose CT scan, MRI attenuation correction scan, or 511-keV transmission scan. If a 511-keV transmission scan is used, the transmission images should be acquired before tracer injection. CT parameters should always be chosen to ensure the lowest doses that are compatible with this purpose are administered to the patient.
The following points relevant to attenuation correction in PET/MRI are to be considered:
-
1.
In PET/MRI, attenuation correction is based on MRI imaging. Thus, MRI-based attenuation correction needs to be accurate and free from artefacts to provide accurate PET quantification.
-
2.
The latest version of MRI attenuation-correction software should be used, including ultrashort echo time (UTE), zero TE (ZTE) sequences, or bone-models for bone detection in brain PET/MRI, where available [16, 17].
-
3.
Various attenuation correction strategies for PET/MRI have been implemented. Some may lead to systematic differences in the activity distribution and calculated semiquantitative metrics (see section Static FET, MET, FDOPA PET) [18] that should carefully be considered during interpretation of PET images [19, 20].
-
4.
MRI attenuation-corrected images must routinely be checked for artefacts, consistency and plausibility during PET/MRI reading. Artefacts on MRI attenuation correction have a direct effect on PET quantification in brain PET/MRI. Typically artefacts may arise from mis-segmentation of brain/fat/bone tissue, or from metallic dental prostheses and metallic implants such as coils, stents, surgical clips, etc. [18, 21, 22]. Artefacts may show as signal voids that exceed the true dimensions of the metal inclusions. Thus, most artefacts are readily detectable on MRI attenuation-corrected images and indicate regions of potentially inaccurate PET quantification [23, 24].
-
5.
Where applicable, time-of-flight PET detection should be used to reduce the impact of metal artefacts in brain PET/MRI examinations [25].
-
6.
Only radiofrequency (RF) head coils labelled for combined PET/MRI use only should be used. Using standard RF head coils labelled for MRI-only use will not be considered in PET/MRI attenuation correction and their use may thus lead to inaccurate PET quantification and artefacts on PET.
-
7.
In longitudinal studies, the patient should always be scanned on the same system using the same procedures to avoid changes related to differences in imaging technology or methodology. In cross-sectional studies, possible differences among scans related to the technologies being used should be considered. Particular care is needed in paediatric patients.
PET comparability
To ensure PET comparability, a standardized protocol for clinical reading should be used with a fixed time for the start of image acquisition.
-
1.
FET: 20 min static image acquisition obtained 20 min after injection. This may be part of a 40–50 min dynamic image acquisition initiated at tracer injection. Dynamic image acquisitions should be started using short frames that progressively increase in duration. From 10 to 50 min after injection 5-min acquisition frames should be used to allow the tracer uptake slope to be assessed during this interval. To allow precise information on the tracer uptake phase to be obtained, the following image acquisition frame sequences could be used during the first 10 min after injection: 12 frames of 5 s, 6 frames of 10 s, 6 frames of 30 s and 5 frames of 60 s.
-
2.
MET: 20 min static image acquisition obtained 10 min after injection.
-
3.
FDOPA: 10–20 min static image acquisition obtained 10–30 min after injection.
-
4.
FDG: 10–20 min static image acquisition obtained at least 45 min after injection.
Movement artefacts
If movement artefacts are expected, it may be helpful to acquire the static time window dynamically, e.g. in 5-min frames, or in list mode. Check the sinograms, and use only those of the properly acquired motion-free time period for reconstruction.
PET image reconstruction
-
1.
During image reconstruction, all corrections for quantitative interpretation are required including attenuation, scatter, random, dead time and decay corrections, as well as detector sensitivity normalization.
-
2.
Time of flight acquisitions and reconstructions are allowed, although the benefit for brain imaging has not yet been fully investigated.
-
3.
Iterative reconstruction is the field standard and should be applied. However, if iterative reconstruction would result in upward bias due to non-negativity constraints applied during reconstruction, filtered back-projection reconstruction may be used as an alternative method.
-
4.
The use of resolution modelling during reconstruction, so-called point-spread-function (PSF) reconstructions, may give rise to Gibbs artefacts and quantitative errors [26], and this method is not recommended.
-
5.
To harmonize PET image quality, the following reconstruction settings/protocols are recommended:
-
(a)
One of the reconstructions should be performed using settings such that the reconstructed images meet EARL requirements for image quality recovery [6], thereby allowing harmonization of PET data for multicentre settings or for use with reference datasets.
-
(b)
As the above harmonizing reconstruction settings will ensure comparable image quality among different generations of PET/CT systems, a higher resolution reconstruction may be desired or required for visual interpretation or tumour delineation. When a specific PET system allows the use of multiple reconstructions, a high-resolution dedicated brain reconstruction protocol may be applied. Such a protocol should preferably meet the following requirements:
-
Voxels size 1–2 mm, but <3 mm in any direction
-
Reconstructed spatial resolution <6 mm full-width at half-maximum
-
-
(a)
Interpretation/quantification
Standardized uptake value calculations and image analysis
General image display
-
1.
PET images should have pixels of at least 16 bits to provide an adequate range of values, and appropriate image scaling should be employed for image display. A colour scale may be used. PET images should be displayed in the transaxial orientation and additionally correlated with morphological images in the coronal and sagittal planes.
-
2.
Internal landmarks can be used for reorientation to achieve a standardized image display. Reorientation procedures based on the intercommissural line are commonly used [27].
-
3.
FET, MET, FDOPA: If the display scale is in colour, it should be adjusted so that the background radioactivity of healthy brain is in the lower third of the range (blue hue in the widely used Sokoloff scale), in order to create standardized conditions for the visual detection of increased tracer accumulation above background.
-
4.
FDG: The display scale should be initially adjusted so that the radioactivity in normal cerebral cortex is near the maximum of the scale. If lesions have higher uptake than the cerebral cortex, the scale should be adjusted such that the lesion with the highest uptake is near to the maximum of the scale. Colour scales with 10 or 20 increments are useful to estimate the relative concentrations of FDG across brain regions and in lesions.
Static FET, MET, FDOPA PET
-
1.
Calculation of the SUV is optional and may be performed by dividing the radioactivity concentration (in kilobecquerels per millilitre) in the tissue by the radioactivity (in megabecquerels) injected per body weight (in kilograms), body surface area (in metres squared) or lean body mass (in kilograms), depending on the most appropriate distribution volume for each tracer.
-
2.
Standard summation images in the ranges defined in section PET comparability (items 1, 2 and 3) are used for clinical reading and should be coregistered and fused with recent high-resolution contrast-enhanced T1-weighted, T2-weighted/FLAIR MRI sequences. Fusion with other MRI sequences is optional. Usually vendor-provided coregistration software solutions are sufficiently robust for clinical use, but must be routinely checked for misalignment during reading. This can be done by adjusting the PET colour scale to clearly visualize the scalp and nose of the patient so that these structures can be compared between the PET and MRI images.
-
3.
In a first visual analysis, qualitative evaluation can be performed and the lesion of interest can be classified as either positive, when tracer uptake visually exceeds the background activity in the contralateral cortex, or negative, when no increased uptake can be seen.
-
4.
MET, FET: In order to ensure intraindividual as well as interindividual comparability, semiquantitative measures of mean and maximal tumour activity uptake values can be calculated as ratios in relation to healthy appearing reference brain tissue (tumour to background ratios, TBRmean and TBRmax, respectively).
-
(a)
The mean physiological brain activity uptake in healthy appearing cortex of the hemisphere contralateral to the tumour including grey and white matter is measured from a large “banana”/crescent-shaped background volume of interest (VOI) [28].
-
(b)
The measurement of TBRmean depends on the delineation of the tumour VOI.
-
(a)
-
5.
FDOPA: Semiquantitative measures of mean and maximal tumour activity uptake values can be calculated as ratios in relation to healthy appearing striatum [29] contralateral to the tumour (tumour to striatum ratios, TSRmean and TSRmax, respectively). The striatum is the most commonly used reference region. Other reference regions have not been investigated systematically.
Static FDG PET
-
1.
A static image acquired for 10–20 min at least 45 min after injection is used for clinical FDG PET reading, and should be coregistered and fused with recent high-resolution contrast-enhanced T1 and T2/FLAIR MRI sequences. Fusion with other MRI sequences is optional.
-
2.
SUVs used directly are generally of limited value in the clinical interpretation of FDG PET neurooncology studies.
-
3.
Qualitative visual analysis can be performed and the lesion of interest can be classified as either positive, when FDG uptake visually exceeds the activity in a reference region (e.g. normal appearing white matter or cerebral cortex), or negative, when FDG uptake in the lesion is less than that in the reference region. Using white matter as the reference region provides better sensitivity for detecting recurrent tumour at the expense of specificity, while using cerebral cortex provides better specificity at the expense of sensitivity.
-
4.
Lesion to reference region ratios using mean or maximum SUV can be used to provide a measure of FDG uptake in lesions. Numerical cut-off values for distinguishing tumour from benign lesions, such as radiation necrosis, and for grading tumours are not well established for FDG. If ratios are used, either white or grey matter rather than a mixture of the two should be used for reference due to the substantially higher FDG uptake in grey matter than in white matter. Additionally, normal-appearing brain should be considered for the reference region to provide consistency across studies.
-
5.
The regional metabolic rate of glucose can be estimated in lesions and normal brain by compartmental modelling or by using graphical analytical approaches. A correction factor, the so-called “lumped constant” [30], can be used to convert the FDG values to values reflecting glucose metabolism [31]. However, little is known about the accuracy of these methods in brain tumours and/or treatment effects. Currently, there is insufficient data to recommend these types of quantitative studies in routine clinical FDG PET for neurooncology.
Cut-off thresholds for definition of biological tumour volume
-
FDG: Not available
-
FET: SUV >1.6–1.8 of the mean value in healthy appearing brain (see section Static FET, MET, FDOPA PET, item 4(a)) [32]
-
MET: SUV >1.3 of the mean value in healthy appearing brain [33]
-
FDOPA: SUV more than the mean value in healthy striatum [29] (not validated histologically)
Dynamic PET acquisition
An established clinical value for dynamic PET acquisitions applies only to FET [7]. Time–activity curves (TAC), i.e. the mean tissue radioactivity in the tumour region of interest (ROI)/VOI (SUV; becquerels per centimetre cubed, counts per centimetre cubed) as a function of time, can be generated from dynamic FET PET images. The TAC of the healthy brain (see section Static FET, MET, FDOPA PET, item 4(a)) should be plotted for comparison to exclude technical artefacts. To extract the TAC of the most aggressive tumour area and to provide sufficient count statistics for curve generation, the following approach is recommended:
-
1.
The VOI is drawn semiautomatically using an individually adapted isocontour of the tumour maximum yielding a volume of 1–2 mL, or using a standard ROI/VOI with a fixed diameter of 1.6 cm centred on the tumour maximum yielding a volume of 2 mL.
-
2.
These ROIs/VOIs can be defined on the summation images of 20–40 min or 10–30 min. The latter may be better suited to the depiction of the early peak uptake in more aggressive gliomas.
-
3.
The shape of the TAC is classified as increasing, decreasing or plateau. For assessment of time to peak (TTP), the time of tumour peak uptake is noted.
Interpretation of static FET/MET/FDOPA PET data
Based on the 2016 WHO classification [34], gliomas will be progressively classified on the basis of histological and molecular characteristics, rather than as low-grade or high-grade gliomas, as follows:
-
1.
Astrocytomas grade II and III (with isocitrate dehydrogenase 1 (IDH1) mutation, without 1p/19q codeletion) [35]
-
2.
Oligodendrogliomas grade II and III (with IDH1 mutation, with 1p/19q codeletion) [36]
-
3.
Wildtype astrocytomas or oligodendrogliomas not otherwise specified
-
4.
Secondary glioblastomas (with IDH1 mutation)
-
5.
Primary glioblastomas (IDH1 wildtype or IDH1-negative) [37, 38]
Available data on the range of radiotracer uptake are limited to FDG, FET and MET [39,40,41,42,43]. Further evidence is required to complement molecular characterization of gliomas and implement radiotracers in the new classification.
-
1.
At primary diagnosis
-
(a)
Negative scan: uptake in the background uptake range or slightly above excludes a grade III/IV glioma, lymphoma or metastasis with high probability. Also, an oligodendroglial tumour is very unlikely. A grade I/II astrocytoma cannot be excluded since approximately 30% exhibit low uptake.
-
(b)
Positive scan: increased uptake has high a positive predictive value for a neoplastic process. A reliable differentiation of grade III/IV and grade I/II gliomas is not possible because of a high proportion of active tumours among the latter, especially in oligodendrogliomas. Local areas with the highest uptake should be used for biopsy guidance.
-
(a)
-
2.
Therapy planning: for FET and MET, areas with uptake higher than the above biological tumour volume (BTV) cut-off activity values are used to delineate the metabolically active tumour tissue for planning of surgery and radiotherapy.
-
3.
Tumour recurrence: increased uptake in the follow-up of previously treated glioma has high accuracy in differentiating treatment-related changes (e.g. pseudoprogression, radionecrosis) from recurrent disease.
-
4.
Therapy monitoring: amino acid uptake progression during different kinds of therapy is indicative of therapy failure, while uptake regression indicates responsiveness. FET and FDOPA PET have been shown to identify pseudoresponse during antiangiogenic therapy.
The TBRmean and TBRmax thresholds for establishing pathological amino acid accumulation depends on the ROI definition technique, the spatial resolution of the PET scan (system type, reconstruction, data filtering) and the clinical question to be answered [44]. The thresholds according to clinical questions are shown in Table 1.
Interpretation of static FDG PET data
-
1.
At primary diagnosis
-
(a)
Increasing FDG uptake by gliomas is correlated with higher grade and worse prognosis [7, 61,62,63,64]. Grade I/II gliomas typically have FDG uptake similar to or less than white matter uptake, although some grade I/II gliomas such as pilocytic astrocytomas have high FDG uptake. Grade III/IV gliomas typically have FDG uptake greater than white matter uptake (see comments on the new WHO classification scheme (see section Interpretation of static FET/MET/FDOPA PET data, item 1).
-
(b)
There is overlap in FDG uptake between grade I/II and grade III/IV gliomas, particularly for gliomas with FDG uptake greater than white matter but less than grey matter uptake. Optimal quantitative thresholds and visual analysis criteria have not been established for definitively distinguishing glioma grade or predicting prognosis based on FDG PET alone.
-
(a)
-
2.
Tumour recurrence
-
(a)
High FDG uptake in enhancing brain lesions is correlated with tumour recurrence. However, high FDG uptake can occur in the brain after radiation therapy including radiation necrosis, and recurrent tumours may have relatively low FDG uptake. Well-defined quantitative and qualitative criteria with high diagnostic accuracy are not available and may not be achievable with FDG PET.
-
(b)
For gliomas treated with radiation therapy, FDG PET can be used to distinguish radiation necrosis from recurrent tumour. Many criteria have been proposed, and wide ranges of sensitivity and specificity have been reported in the literature [65,66,67,68,69,70,71]. A reasonable approach is to use normal white and grey matter as the reference regions. Lesions with FDG uptake similar to or less than white matter uptake are probably radiation necrosis while lesions with FDG uptake higher than grey matter uptake are probably recurrent tumour. Lesions with FDG uptake higher than white matter but less than grey matter uptake may be radiation necrosis, recurrent tumour or a mixture of both. Correlation with MRI, the presence of focal uptake suggesting recurrence within a larger region of diffuse lower level FDG uptake, and the clinical presentation may be useful in these cases.
-
(c)
The choice of the quantitative cut-off value or visual reference region will affect the sensitivity and specificity of the results. For example, using normal white matter as the reference region and categorizing lesion with FDG uptake similar to or less than white matter uptake as radiation necrosis and lesions with uptake higher than normal white matter uptake as recurrent tumour will provide higher sensitivity (negative imaging more likely to be treatment effect) at the expense of specificity (positive imaging more likely to be false positive). Similarly, using normal grey matter as the reference region will provide lower sensitivity (negative imaging more likely to be false-negative) with an increase in specificity (positive imaging more likely to be recurrent tumour).
-
(a)
Interpretation of dynamic FET PET data
-
1.
An early peak in the TAC shape of the mean ROI/VOI activity (<20 min after injection) followed by a plateau or a decreasing TAC is indicative of a grade III/IV tumour.
-
2.
Continuously increasing uptake up to 40 min after injection is more frequently observed in grade I/II gliomas, but is not specific. This TAC pattern is also typical of treatment-induced changes, e.g. radionecrosis, pseudoprogression.
-
3.
A change in the TAC pattern during follow-up of grade I/II gliomas from an increasing TAC to an early peak with a decreasing TAC is indicative of malignant transformation [54].
Physiological tracer distribution
-
FDG
-
1.
Common: high physiological uptake in grey matter (e.g. cerebral and cerebellar cortex, deep grey nuclei).
-
2.
Common: moderate uptake in the extraocular muscles.
-
3.
Occasionally: brain activation during the uptake phase such as patient motion or visual stimulation can result in higher uptake in the associated regions in the cerebral cortex.
-
1.
-
FET, MET [72]
-
1.
Common: slight uptake in vascular structures, basal ganglia, cerebellum, skin and salivary glands.
-
2.
Occasionally: slight focal uptake in pineal body, choroid plexus and clivus bone marrow.
-
1.
-
FDOPA
-
1.
Common: moderately increased uptake in basal ganglia and pituitary, and slight uptake in the cerebellum, skin, optic nerve, ocular muscles and salivary glands.
-
2.
Occasionally: pineal body.
-
3.
No increased uptake in vascular structures.
-
1.
Known pitfalls
-
All tracers
-
1.
Uptake may be increased in inflammatory lesions and epileptic seizures.
-
2.
Uptake may be underestimated in small lesions relative to image resolution.
-
1.
-
FDG
-
1.
High uptake in grey matter can obscure lesions within or adjacent to grey matter.
-
2.
High blood glucose levels at the time of injection decrease uptake in tumour and healthy appearing grey matter, but may not affect lesion detection.
-
3.
Perivascular infiltration.
-
4.
Anatomical abnormalities.
-
5.
Treatment effects may decrease uptake in the treatment area and brain regions that receive synaptic input from the treated area (diaschisis).
-
1.
-
MET, FET, FDOPA
-
1.
TBRmean, TBRmax and BTV may be overestimated if there is reduced uptake in the reference brain tissue VOI because of structural changes, e.g. atrophy, trauma and infarcts, or reduced tracer delivery. e.g. ischaemia.
-
2.
As MET, FET, and FDOPA are all transported across the blood–brain barrier and into cells by system L amino acid transport, they can all be expected to have similar pitfalls (Table 2).
-
1.
-
Dynamic FET
-
1.
In early images, up to 15 min after injection, blood pool uptake is relatively high, and tracer activity in vascular structures may have the same appearance as tumour tissue uptake.
-
2.
Reduced uptake in occipital and temporal skin areas may be seen in static images, probably as a result of reduced perfusion caused by the head padding.
-
3.
An increasing TAC may indicate inflammatory lesions.
-
4.
A decreasing TAC may be seen in WHO grade II oligodendroglial tumours (around 50%).
-
5.
A decreasing TAC may be seen in tumours close to sinuses because of the influence of venous blood activity.
-
6.
After antiangiogenic treatment the TAC may change from a decreasing to an increasing pattern.
-
1.
Documentation and reporting
Description of findings in brain tumour imaging should generally comply with previously published guidelines for FDG imaging in oncology and with regard to general aspects of reporting such as due diligence [6].
The content of the report affects patient management and clinical outcomes, and is a legal document. It is good practice to provide a structured report with concise concluding statements intended to answer the specific clinical question(s) posed, if possible.
Regardless of the radiotracer, reports should follow the general structure outlined below.
General information
-
1.
Name of the patient and other identifiers, such as date of birth.
-
2.
Name of the referring physician.
-
3.
Type and date of examination.
-
4.
Radiopharmaceutical including route of administration and amount of activity administered.
-
5.
Patient history with emphasis on diagnosis and tumour-related treatment and the clinical question leading to the study request (see sections Common clinical indications and Request).
Body of the report
-
1.
Procedure description
-
(a)
Information on the imaging procedure (e.g. static or dynamic scan), and time between PET tracer injection and image acquisition.
-
(b)
If FDG is used, the measured blood glucose level at the time of injection.
-
(c)
If sedation is performed, type and time of medication in relation to the tracer injection.
-
(d)
If a low-dose CT scan is performed for attenuation correction, a statement such as “not performed for diagnostic purposes, not replacing diagnostic CT” could be added.
-
(e)
The use of a nonconventional system type (e.g. PET/MRI) should be mentioned.
-
(a)
-
2.
Data quality
-
(a)
Abnormal tracer biodistribution.
-
(b)
CT-related artefacts, e.g. from metallic implants.
-
(c)
Poor compliance with fasting.
-
(d)
Any observed events that may adversely influence interpretation, e.g. head movements, seizure activity.
-
(e)
If FDG is used, increased blood glucose level.
-
(a)
-
3.
Comparative data
-
(a)
PET images should be compared with morphological data, particular MRI data, whenever possible.
-
(b)
PET images should be compared with previous PET scans to evaluate the course of disease.
-
(c)
The type and date of comparative data should be noted before description of the imaging findings.
-
(a)
-
4.
Description of findings
-
(a)
The normality of radiotracer uptake should be stated, whether normal or abnormal.
-
(b)
In case of abnormal findings, the location (with a correct anatomical description), extent and intensity of pathological tracer accumulation in relation to normal tissue uptake should be described.
-
(c)
Uptake characteristics, including:
-
Shape of uptake, e.g. focal, diffuse, inhomogeneous.
-
Intensity of uptake in relation to healthy brain uptake (slight, moderate or strong).
-
Extent and peak uptake, in correlation with, for example, T1 contrast enhancement and/or T2/FLAIR hyperintensity on MRI or obvious anatomical abnormalities on CT/low-dose CT images.
-
-
(d)
Semiquantitative parameters
-
Calculate and report the TBRmax. Reporting the TBRmean and BTV is optional. Determination of FDG SUV/SUV ratio, TBRmean, TBRmax and BTV are optional in the clinical setting and do not have well-established utility in characterizing gliomas or distinguishing treatment effects from recurrence.
-
When dynamic imaging is performed with FET, the pattern of the tumour TAC (increasing, decreasing, plateau) should be described. The reporting of TTP and slope is optional.
-
-
(e)
Clinically relevant incidental findings should be reported, e.g. extracerebral metastases.
-
(f)
Comparison with previously performed PET studies, e.g. for therapy response or malignant transformation.
-
(a)
-
5.
Limitations:
when appropriate, factors that could have limited data quality or diagnostic accuracy should be mentioned (Table 2).
Interpretation
The interpretation should address the question raised in the clinical request and integrate medical history, comparative imaging and any limitations. A precise diagnosis should be given whenever possible. Additional scans or follow-up scans should be recommended when appropriate.
Equipment specifications
System specifications
The use of state-of-the-art 3D PET/CT or PET/MRI systems is recommended. The system should allow collection of low-dose CT images or MRI-based sequences that can be used for attenuation and scatter correction of the PET emission data. A dedicated brain PET-only system may be used provided it is equipped with transmission scan sources of sufficient strength – as recommended by the manufacturer – to ensure sufficient quality of the transmission scans and thereby of the PET emission data attenuation correction. PET(/CT) systems should have a minimal axial field of view of 15 cm to ensure sufficient coverage of the entire brain, including cerebellum and brainstem.
PET acquisition
The system should be able to acquire both static and dynamic or list-mode PET emission data in 3D mode. Data should be reconstructed online or offline (i.e. retrospectively) in single or multiple frames, as specified by the study protocols and these guidelines. In addition, PET images should be able to be reconstructed with and without attenuation correction. The PET images without attenuation correction should not be used for primary interpretation but can be useful for recognizing attenuation artefacts in the attenuation-corrected PET images. The system should have all functionalities and methods available as required for quantitative brain PET imaging and reconstruction, including, but not limited to, online randoms correction, scatter correction, attenuation correction, dead time correction, decay and abundance correction and normalization (correction for detector sensitivities).
Quality control and improvement
Quality control and interinstitutional PET system performance harmonization
Various factors affecting PET image quality and quantification have previously been reviewed [91]. Although this review focused on the use of radiolabelled amino acids and FDG for glioma imaging, the technical and imaging physics uncertainties indicated in that review are valid for any PET examination regardless of radiotracer or specific application. The use of brain PET examinations in multicentre studies and/or when data are compared with a reference database or disease pattern, it is of the utmost importance that PET data are collected in such a manner that they can be pooled and compared. In order to guarantee sufficient image quality, quantitative performance and image harmonization, the performance of the PET systems must be regularly checked by several QC experiments. All regular and vendor-provided maintenance and QC procedures should be followed. QC experiments should at least address the following:
-
Daily check of detector performance, i.e. with point, rod or cylindrical sources to automatically test and visualize the proper functioning of detector modules including inspection of 2D sinograms.
-
Daily check of PET activity concentration measurement calibration using an activity filled cylindrical phantom source following the procedure recommended by the manufacturer.
-
Cross-calibration of the PET(/CT) system against the locally used dose calibrator to prepare and measure patient-specific radiotracer activities. Cross-calibrations should be performed following EARL recommendations and criteria.
-
Correct alignment between PET and CT should be verified according to the procedure and frequency recommended by the manufacturer.
-
Additional QC procedures performed less frequently following the instructions provided by the manufacturer and the EANM recommendations for routine QC of nuclear medicine equipment [92].
CT quality control
The EU guidelines for FDG PET/CT tumour imaging discuss several documents and reports that have been published on CT quality control (CT-QC). For example, an overview of CT-QC is given in the “Equipment Specifications” and “Quality Control” sections of the following American College of Radiology (ACR) practice parameters: “ACR–ASNR–SPR Practice parameter for the performance of Computed Tomography (CT) of the extracranial head and neck” (https://www.acr.org/-/media/ACR/Files/Practice-Parameters/CT-Head-Neck.pdf?la=en), “ACR–SCBT-MR–SPR–STR Practice parameter for the performance of thoracic computed tomography (CT)” (https://www.acr.org/-/media/ACR/Files/Practice-Parameters/CT-Thoracic.pdf?la=en), and “ACR–SPR Practice parameter for the performance of thoracic Computed Tomography (CT) of the abdomen and Computed Tomography (CT) of the Pelvis”, (https://www.acr.org/-/media/ACR/Files/Practice-Parameters/CT-Abd-Pel.pdf?la=en). CT-QC is also the subject of the Institute of Physics and Engineering in Medicine (IPEM) report 91 “Recommended Standards for the Routine Performance Testing of Diagnostic X-Ray Systems”. In addition, CT performance monitoring guidelines are given in the American College of Radiology: ”ACR–AAPM Technical standards for diagnostic medical physics performance monitoring of Computed Tomography (CT) Equipment”, (https://www.acr.org/-/media/ACR/Files/Practice-Parameters/CT-Equip.pdf?la=en).
MR quality control in PET/MRI
While there are no regulatory requirements for special/standard QC/QA procedures for MRI systems, numerous points should be considered for conducting safe and high-quality MRI examinations as outlined in section Examination procedures/specifications. It is advisable to adhere to the recommendations of the manufacturer (i.e. follow the planned maintenance intervals). For PET/MRI systems an approach to basic MRI QC to be performed by the user is described in a review by Sattler et al. [93].
Radiation safety
The systemic use of radiotracers leads to systemic exposure of the patients to radiation. The amounts of radioactivity usually delivered with the administration of 11C-labelled and 18F-labelled PET radioligands (see section Administered activity in adults) result in effective doses (ED) of the same order of magnitude as delivered by other 11C-labelled and 18F-labelled radiotracers [94]. The radiation dose from low-dose CT scans of the head region depends on the CT scanning parameters and is generally well below 0.5 mSv. The overall ED from PET/CT investigations of the head region, when accounting for the whole-body exposure, should remain near or below 5 mSv. In adults, the organ with the highest radiation dose for all the above tracers is the urinary bladder wall (Table 3).
Conclusion
Since the previous EANM guidelines in 2006 [10], the clinical use of molecular imaging with PET and PET/CT in the diagnosis of glioma has continuously increased in Europe and the US. For successful and appropriate use of this technology, a clear understanding of the capabilities and limitations of the technology and appropriate patient selection, preparation, scan acquisition and image reconstruction are required. This document attempts to provide some guidance on the performance and interpretation of molecular imaging to supplement recent clinical guidelines [7], and to bring PET brain imaging into daily clinical practice and into larger scale interinstitutional clinical neurooncological trials across imaging platforms.
References
Ostrom QT, Gittleman H, Fulop J, Liu M, Blanda R, Kromer C, et al. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2008-2012. Neuro Oncol. 2015;17(Suppl 4):iv1–iv62.
Weller M, van den Bent M, Tonn JC, Stupp R, Preusser M, Cohen-Jonathan-Moyal E, et al. European Association for Neuro-Oncology (EANO) guideline on the diagnosis and treatment of adult astrocytic and oligodendroglial gliomas. Lancet Oncol. 2017;18:e315–29.
Reardon DA, Ballman KV, Buckner JC, Chang SM, Ellingson BM. Impact of imaging measurements on response assessment in glioblastoma clinical trials. Neuro Oncol. 2014;16(Suppl 7):vii24–35.
Okada H, Weller M, Huang R, Finocchiaro G, Gilbert MR, Wick W, et al. Immunotherapy response assessment in neuro-oncology: a report of the RANO working group. Lancet Oncol. 2015;16:e534–42.
Wen PY, Macdonald DR, Reardon DA, Cloughesy TF, Sorensen AG, Galanis E, et al. Updated response assessment criteria for high-grade gliomas: Response Assessment in Neuro-Oncology Working Group. J Clin Oncol. 2010;28:1963–72.
Boellaard R, Delgado-Bolton R, Oyen WJ, Giammarile F, Tatsch K, Eschner W, et al. FDG PET/CT: EANM procedure guidelines for tumour imaging: version 2.0. Eur J Nucl Med Mol Imaging. 2015;42:328–54.
Albert NL, Weller M, Suchorska B, Galldiks N, Soffietti R, Kim MM, et al. Response Assessment in Neuro-Oncology Working Group and European Association for Neuro-Oncology recommendations for the clinical use of PET imaging in gliomas. Neuro Oncol. 2016;18:1199–208.
Langen KJ, Galldiks N, Hattingen E, Shah NJ. Advances in neuro-oncology imaging. Nat Rev Neurol. 2017;13:279–89.
Langen KJ, Watts C. Neuro-oncology: amino acid PET for brain tumours - ready for the clinic. Nat Rev Neurol. 2016;12:375–6.
Vander Borght T, Asenbaum S, Bartenstein P, Halldin C, Kapucu Ö, Van Laere K, et al. EANM procedure guidelines for brain tumour imaging using labelled amino acid analogues. Eur J Nucl Med Mol Imaging. 2006;33:1374–80.
Fragoso Costa P, Santos A, Testanera G. An insight into the EANM Technologist Committee benchmark document on nuclear medicine technologists’ competencies. Eur J Nucl Med Mol Imaging. 2017;44:1604–6.
Waxman AD, Herholz K, Lewis DH, Herscovitch P, Minoshima S, Ichise M, et al. Society of Nuclear Medicine Procedure Guideline for FDG PET Brain Imaging Version 1.0. Reston, VA: Society of Nuclear Medicine; 2009. p. 1–12.
Varrone A, Asenbaum S, Vander Borght T, Booij J, Nobili F, Någren K, et al. EANM procedure guidelines for PET brain imaging using [(18)F]FDG, version 2. Eur J Nucl Med Mol Imaging. 2009;36:2103–10.
Shellock FG. Reference manual for magnetic resonance safety, implants, and devices: edition 2018. Biomedical Research Publishing Group; 2018.
Lassmann M, Biassoni L, Monsieurs M, Franzius C, Jacobs F, EANM Dosimetry and Paediatrics Committees. The new EANM paediatric dosage card. Eur J Nucl Med Mol Imaging. 2007;34:796–8.
Koesters T, Friedman KP, Fenchel M, Zhan Y, Hermosillo G, Babb J, et al. Dixon sequence with superimposed model-based bone compartment provides highly accurate PET/MR attenuation correction of the brain. J Nucl Med. 2016;57:918–24.
Bailey DL, Pichler BJ, Gückel B, Antoch G, Barthel H, Bhujwalla ZM, et al. Combined PET/MRI: global warming—summary report of the 6th International Workshop on PET/MRI, March 27-29, 2017, Tübingen, Germany. Mol Imaging Biol. 2018;20:4–20.
Ladefoged CN, Andersen FL, Kjær A, Højgaard L, Law I. RESOLUTE PET/MRI attenuation correction for O-(2-18F-fluoroethyl)-L-tyrosine (FET) in brain tumor patients with metal implants. Front Neurosci. 2017;11:453.
Andersen FL, Ladefoged CN, Beyer T, Keller SH, Hansen AE, Højgaard L, et al. Combined PET/MR imaging in neurology: MR-based attenuation correction implies a strong spatial bias when ignoring bone. Neuroimage. 2014;84:206–16.
Ladefoged CN, Law I, Anazodo U, St Lawrence K, Izquierdo-Garcia D, Catana C, et al. A multi-centre evaluation of eleven clinically feasible brain PET/MRI attenuation correction techniques using a large cohort of patients. Neuroimage. 2017;147:346–59.
Ladefoged CN, Hansen AE, Keller SH, Holm S, Law I, Beyer T, et al. Impact of incorrect tissue classification in Dixon-based MR-AC: fat-water tissue inversion. EJNMMI Phys. 2014;1:101.
Ladefoged CN, Hansen AE, Keller SH, Fischer BM, Rasmussen JH, Law I, et al. Dental artifacts in the head and neck region: implications for Dixon-based attenuation correction in PET/MR. EJNMMI Phys. 2015;2:8.
Brendle C, Schmidt H, Oergel A, Bezrukov I, Mueller M, Schraml C, et al. Segmentation-based attenuation correction in positron emission tomography/magnetic resonance: erroneous tissue identification and its impact on positron emission tomography interpretation. Invest Radiol. 2015;50:339–46.
Fuin N, Pedemonte S, Catalano OA, Izquierdo-Garcia D, Soricelli A, Salvatore M, et al. PET/MRI in the presence of metal implants: completion of the attenuation map from PET emission data. J Nucl Med. 2017;58:840–5.
Ter Voert EEGW, Veit-Haibach P, Ahn S, Wiesinger F, Khalighi MM, Levin CS, et al. Clinical evaluation of TOF versus non-TOF on PET artifacts in simultaneous PET/MR: a dual centre experience. Eur J Nucl Med Mol Imaging. 2017;44:1223–33.
Munk OL, Tolbod LP, Hansen SB, Bogsrud TV. Point-spread function reconstructed PET images of sub-centimeter lesions are not quantitative. EJNMMI Phys. 2017;4:5.
Minoshima S, Koeppe RA, Mintun MA, Berger KL, Taylor SF, Frey KA, et al. Automated detection of the intercommissural line for stereotactic localization of functional brain images. J Nucl Med. 1993;34:322–9.
Unterrainer M, Vettermann F, Brendel M, Holzgreve A, Lifschitz M, Zähringer M, et al. Towards standardization of (18)F-FET PET imaging: do we need a consistent method of background activity assessment. EJNMMI Res. 2017;7:48.
Schwarzenberg J, Czernin J, Cloughesy TF, Ellingson BM, Pope WB, Grogan T, et al. Treatment response evaluation using 18F-FDOPA PET in patients with recurrent malignant glioma on bevacizumab therapy. Clin Cancer Res. 2014;20:3550–9.
Graham MM, Muzi M, Spence AM, O'Sullivan F, Lewellen TK, Link JM, et al. The FDG lumped constant in normal human brain. J Nucl Med. 2002;43:1157–66.
Lucignani G, Schmidt KC, Moresco RM, Striano G, Colombo F, Sokoloff L, et al. Measurement of regional cerebral glucose utilization with fluorine-18-FDG and PET in heterogeneous tissues: theoretical considerations and practical procedure. J Nucl Med. 1993;34:360–9.
Pauleit D, Floeth F, Hamacher K, Riemenschneider MJ, Reifenberger G, Müller HW, et al. O-(2-[18F]fluoroethyl)-L-tyrosine PET combined with MRI improves the diagnostic assessment of cerebral gliomas. Brain. 2005;128:678–87.
Kracht LW, Miletic H, Busch S, Jacobs AH, Voges J, Hoevels M, et al. Delineation of brain tumor extent with [11C]L-methionine positron emission tomography: local comparison with stereotactic histopathology. Clin Cancer Res. 2004;10:7163–70.
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016;131:803–20.
Suchorska B, Giese A, Biczok A, Unterrainer M, Weller M, Drexler M, et al. Identification of time-to-peak on dynamic 18F-FET-PET as a prognostic marker specifically in IDH1/2 mutant diffuse astrocytoma. Neuro Oncol. 2018;20:279–88.
Jansen NL, Schwartz C, Graute V, Eigenbrod S, Lutz J, Egensperger R, et al. Prediction of oligodendroglial histology and LOH 1p/19q using dynamic [(18)F]FET-PET imaging in intracranial WHO grade II and III gliomas. Neuro Oncol. 2012;14:1473–80.
Verger A, Stoffels G, Bauer EK, Lohmann P, Blau T, Fink GR, et al. Static and dynamic (18)F-FET PET for the characterization of gliomas defined by IDH and 1p/19q status. Eur J Nucl Med Mol Imaging. 2018;45:443–51.
Lopci E, Riva M, Olivari L, Raneri F, Soffietti R, Piccardo A, et al. Prognostic value of molecular and imaging biomarkers in patients with supratentorial glioma. Eur J Nucl Med Mol Imaging. 2017;44:1155–64.
Saito T, Maruyama T, Muragaki Y, Tanaka M, Nitta M, Shinoda J, et al. 11C-Methionine uptake correlates with combined 1p and 19q loss of heterozygosity in oligodendroglial tumors. AJNR Am J Neuroradiol. 2013;34:85–91.
Niyazi M, Schnell O, Suchorska B, Schwarz SB, Ganswindt U, Geisler J, et al. FET-PET assessed recurrence pattern after radio-chemotherapy in newly diagnosed patients with glioblastoma is influenced by MGMT methylation status. Radiother Oncol. 2012;104:78–82.
Okita Y, Nonaka M, Shofuda T, Kanematsu D, Yoshioka E, Kodama Y, et al. (11)C-methinine uptake correlates with MGMT promoter methylation in nonenhancing gliomas. Clin Neurol Neurosurg. 2014;125:212–6.
Choi H, Bang JI, Cheon GJ, Kim YH, Park CK, Park SH, et al. 18F-fluorodeoxyglucose and 11C-methionine positron emission tomography in relation to methyl-guanine methyltransferase promoter methylation in high-grade gliomas. Nucl Med Commun. 2015;36:211–8.
Bette S, Gempt J, Delbridge C, Kirschke JS, Schlegel J, Foerster S, et al. Prognostic value of O-(2-[18F]-fluoroethyl)-L-tyrosine-positron emission tomography imaging for histopathologic characteristics and progression-free survival in patients with low-grade glioma. World Neurosurg. 2016;89:230–9.
Filss CP, Albert NL, Böning G, Kops ER, Suchorska B, Stoffels G, et al. O-(2-[(18)F]fluoroethyl)-L-tyrosine PET in gliomas: influence of data processing in different centres. EJNMMI Res. 2017;7:64.
Rapp M, Heinzel A, Galldiks N, Stoffels G, Felsberg J, Ewelt C, et al. Diagnostic performance of 18F-FET PET in newly diagnosed cerebral lesions suggestive of glioma. J Nucl Med. 2013;54:229–35.
Herholz K, Holzer T, Bauer B, Schröder R, Voges J, Ernestus RI, et al. 11C-methionine PET for differential diagnosis of low-grade gliomas. Neurology. 1998;50:1316–22.
Lohmann P, Herzog H, Rota Kops E, Stoffels G, Judov N, Filss C, et al. Dual-time-point O-(2-[F]fluoroethyl)-L-tyrosine PET for grading of cerebral gliomas. Eur Radiol. 2015;25:3017–24.
Albert NL, Winkelmann I, Suchorska B, Wenter V, Schmid-Tannwald C, Mille E, et al. Early static F-FET-PET scans have a higher accuracy for glioma grading than the standard 20-40 min scans. Eur J Nucl Med Mol Imaging. 2016;43:1105–14.
Galldiks N, Ullrich R, Schroeter M, Fink GR, Kracht LW. Volumetry of [(11)C]-methionine PET uptake and MRI contrast enhancement in patients with recurrent glioblastoma multiforme. Eur J Nucl Med Mol Imaging. 2010;37:84–92.
Pafundi DH, Laack NN, Youland RS, Parney IF, Lowe VJ, Giannini C, et al. Biopsy validation of 18F-DOPA PET and biodistribution in gliomas for neurosurgical planning and radiotherapy target delineation: results of a prospective pilot study. Neuro Oncol. 2013;15:1058–67.
Galldiks N, Stoffels G, Filss C, Rapp M, Blau T, Tscherpel C, et al. The use of dynamic O-(2-18F-fluoroethyl)-l-tyrosine PET in the diagnosis of patients with progressive and recurrent glioma. Neuro Oncol. 2015;17:1293–300.
Terakawa Y, Tsuyuguchi N, Iwai Y, Yamanaka K, Higashiyama S, Takami T, et al. Diagnostic accuracy of 11C-methionine PET for differentiation of recurrent brain tumors from radiation necrosis after radiotherapy. J Nucl Med. 2008;49:694–9.
Herrmann K, Czernin J, Cloughesy T, Lai A, Pomykala KL, Benz MR, et al. Comparison of visual and semiquantitative analysis of 18F-FDOPA-PET/CT for recurrence detection in glioblastoma patients. Neuro Oncol. 2014;16:603–9.
Galldiks N, Stoffels G, Ruge MI, Rapp M, Sabel M, Reifenberger G, et al. Role of O-(2-18F-fluoroethyl)-L-tyrosine PET as a diagnostic tool for detection of malignant progression in patients with low-grade glioma. J Nucl Med. 2013;54:2046–54.
Galldiks N, Dunkl V, Stoffels G, Hutterer M, Rapp M, Sabel M, et al. Diagnosis of pseudoprogression in patients with glioblastoma using O-(2-[(18)F]fluoroethyl)-L-tyrosine PET. Eur J Nucl Med Mol Imaging. 2015;42:685–95.
Kebir S, Fimmers R, Galldiks N, Schäfer N, Mack F, Schaub C, et al. Late pseudoprogression in glioblastoma: diagnostic value of dynamic O-(2-[18F]fluoroethyl)-L-tyrosine PET. Clin Cancer Res. 2016;22:2190–6.
Galldiks N, Langen KJ, Holy R, Pinkawa M, Stoffels G, Nolte KW, et al. Assessment of treatment response in patients with glioblastoma using O-(2-18F-fluoroethyl)-L-tyrosine PET in comparison to MRI. J Nucl Med. 2012;53:1048–57.
Hutterer M, Nowosielski M, Putzer D, Waitz D, Tinkhauser G, Kostron H, et al. O-(2-18F-fluoroethyl)-L-tyrosine PET predicts failure of antiangiogenic treatment in patients with recurrent high-grade glioma. J Nucl Med. 2011;52:856–64.
Galldiks N, Rapp M, Stoffels G, Fink GR, Shah NJ, Coenen HH, et al. Response assessment of bevacizumab in patients with recurrent malignant glioma using [(18)F]fluoroethyl-L-tyrosine PET in comparison to MRI. Eur J Nucl Med Mol Imaging. 2013;40:22–33.
Galldiks N, Kracht LW, Burghaus L, Thomas A, Jacobs AH, Heiss WD, et al. Use of (11)C-methionine PET to monitor the effects of temozolomide chemotherapy in malignant gliomas. Eur J Nucl Med Mol Imaging. 2006;33:516–24.
Colavolpe C, Chinot O, Metellus P, Mancini J, Barrie M, Bequet-Boucard C, et al. FDG-PET predicts survival in recurrent high-grade gliomas treated with bevacizumab and irinotecan. Neuro Oncol. 2012;14:649–57.
De Witte O, Lefranc F, Levivier M, Salmon I, Brotchi J, Goldman S. FDG-PET as a prognostic factor in high-grade astrocytoma. J Neurooncol. 2000;49:157–63.
Dunet V, Pomoni A, Hottinger A, Nicod-Lalonde M, Prior JO. Performance of 18F-FET versus 18F-FDG-PET for the diagnosis and grading of brain tumors: systematic review and meta-analysis. Neuro Oncol. 2016;18:426–34.
Mertens K, Acou M, Van Hauwe J, De Ruyck I, Van den Broecke C, Kalala JP, et al. Validation of 18F-FDG PET at conventional and delayed intervals for the discrimination of high-grade from low-grade gliomas: a stereotactic PET and MRI study. Clin Nucl Med. 2013;38:495–500.
Dankbaar JW, Snijders TJ, Robe PA, Seute T, Eppinga W, Hendrikse J, et al. The use of (18)F-FDG PET to differentiate progressive disease from treatment induced necrosis in high grade glioma. J Neurooncol. 2015;125:167–75.
Imani F, Boada FE, Lieberman FS, Davis DK, Mountz JM. Molecular and metabolic pattern classification for detection of brain glioma progression. Eur J Radiol. 2014;83:e100–5.
Nihashi T, Dahabreh IJ, Terasawa T. Diagnostic accuracy of PET for recurrent glioma diagnosis: a meta-analysis. AJNR Am J Neuroradiol. 2013;34:944–50.
Nihashi T, Dahabreh IJ, Terasawa T. PET in the clinical management of glioma: evidence map. AJR Am J Roentgenol. 2013;200:W654–60.
Santra A, Kumar R, Sharma P, Bal C, Kumar A, Julka PK, et al. F-18 FDG PET-CT in patients with recurrent glioma: comparison with contrast enhanced MRI. Eur J Radiol. 2012;81:508–13.
Chen W. Clinical applications of PET in brain tumors. J Nucl Med. 2007;48:1468–81.
Wray R, Solnes L, Mena E, Meoded A, Subramaniam RM. (18)F-Flourodeoxy-glucose PET/computed tomography in brain tumors: value to patient management and survival outcomes. PET Clin. 2015;10:423–30.
Cook GJ, Maisey MN, Fogelman I. Normal variants, artefacts and interpretative pitfalls in PET imaging with 18-fluoro-2-deoxyglucose and carbon-11 methionine. Eur J Nucl Med. 1999;26:1363–78.
Dethy S, Manto M, Kentos A, Konopnicki D, Pirotte B, Goldman S, et al. PET findings in a brain abscess associated with a silent atrial septal defect. Clin Neurol Neurosurg. 1995;97:349–53.
Floeth FW, Pauleit D, Sabel M, Reifenberger G, Stoffels G, Stummer W, et al. 18F-FET PET differentiation of ring-enhancing brain lesions. J Nucl Med. 2006;47:776–82.
Pichler R, Dunzinger A, Wurm G, Pichler J, Weis S, Nussbaumer K, et al. Is there a place for FET PET in the initial evaluation of brain lesions with unknown significance? Eur J Nucl Med Mol Imaging. 2010;37:1521–8.
Tsuyuguchi N, Sunada I, Ohata K, Takami T, Nishio A, Hara M, et al. Evaluation of treatment effects in brain abscess with positron emission tomography: comparison of fluorine-18-fluorodeoxyglucose and carbon-11-methionine. Ann Nucl Med. 2003;17:47–51.
Ogawa T, Hatazawa J, Inugami A, Murakami M, Fujita H, Shimosegawa E, et al. Carbon-11-methionine PET evaluation of intracerebral hematoma: distinguishing neoplastic from non-neoplastic hematoma. J Nucl Med. 1995;36:2175–9.
Dethy S, Goldman S, Blecic S, Luxen A, Levivier M, Hildebrand J. Carbon-11-methionine and fluorine-18-FDG PET study in brain hematoma. J Nucl Med. 1994;35:1162–6.
Salber D, Stoffels G, Oros-Peusquens AM, Shah NJ, Reifenberger G, Hamacher K, et al. Comparison of O-(2-18F-fluoroethyl)-L-tyrosine and L-3H-methionine uptake in cerebral hematomas. J Nucl Med. 2010;51:790–7.
Zazulia AR, Videen TO, Powers WJ. Transient focal increase in perihematomal glucose metabolism after acute human intracerebral hemorrhage. Stroke. 2009;40:1638–43.
Jacobs A. Amino acid uptake in ischemically compromised brain tissue. Stroke. 1995;26:1859–66.
Salber D, Stoffels G, Pauleit D, Reifenberger G, Sabel M, Shah NJ, et al. Differential uptake of [18F]FET and [3H]l-methionine in focal cortical ischemia. Nucl Med Biol. 2006;33:1029–35.
Law I, Borgwardt L, Højgaard L. Pediatric hybrid imaging of the brain. In: von Schulthess GK, editor. Clinical molecular anatomic imaging - PET/CT, PET/MR and SPECT/CT. Zürich: Wolters Kluwer Health; 2015. p. 218–29.
Morana G, Piccardo A, Garrè ML, Cabria M, Rossi A. 18F-DOPA uptake of developmental venous anomalies in children with brain tumors. Clin Nucl Med. 2016;41:e351–2.
Schiepers C, Van Hecke P, Vandenberghe R, Van Oostende S, Dupont P, Demaerel P, et al. Positron emission tomography, magnetic resonance imaging and proton NMR spectroscopy of white matter in multiple sclerosis. Mult Scler. 1997;3:8–17.
Singhal T, Narayanan TK, Jain V, Mukherjee J, Mantil J. 11C-L-methionine positron emission tomography in the clinical management of cerebral gliomas. Mol Imaging Biol. 2008;10:1–18.
Jansen NL, Suchorska B, Schwarz SB, Eigenbrod S, Lutz J, Graute V, et al. [18F]fluoroethyltyrosine-positron emission tomography-based therapy monitoring after stereotactic iodine-125 brachytherapy in patients with recurrent high-grade glioma. Mol Imaging. 2013;12:137–47.
Hutterer M, Ebner Y, Riemenschneider MJ, Willuweit A, McCoy M, Egger B, et al. Epileptic activity increases cerebral amino acid transport assessed by [18F]-fluoroethyl-L-tyrosine amino acid PET: a potential brain tumor mimic. J Nucl Med. 2017;58:129–37.
Lopci E, Bello L, Chiti A. (11)C-methionine uptake in secondary brain epilepsy. Rev Esp Med Nucl Imagen Mol. 2014;33:234–6.
Novak L, Molnar P, Lengyel Z, Tron L. Does increased 18FDG uptake reflect malignant transformation of a low-grade glioma? A diagnostic dilemma. Neurol India. 2005;53:112–4.
Boellaard R, O’Doherty MJ, Weber WA, Mottaghy FM, Lonsdale MN, Stroobants SG, et al. FDG PET and PET/CT: EANM procedure guidelines for tumour PET imaging: version 1.0. Eur J Nucl Med Mol Imaging. 2010;37:181–200.
On behalf of the EANM Physics Committee: Busemann Sokole E, Płachcínska A, Britten A, et al. Routine quality control recommendations for nuclear medicine instrumentation. Eur J Nucl Med Mol Imaging. 2010;37:662–71.
Sattler B, Jochimsen T, Barthel H, Sommerfeld K, Stumpp P, Hoffmann KT, et al. Physical and organizational provision for installation, regulatory requirements and implementation of a simultaneous hybrid PET/MR-imaging system in an integrated research and clinical setting. MAGMA. 2013;26:159–71.
Zanotti-Fregonara P, Lammertsma AA, Innis RB. Suggested pathway to assess radiation safety of 18F-labeled PET tracers for first-in-human studies. Eur J Nucl Med Mol Imaging. 2013;40:1781–3.
Mattsson S, Johansson L, Leide Svegborn S, Liniecki J, Noßke D, Riklund KÅ, et al. Radiation dose to patients from radiopharmaceuticals: a compendium of current information related to frequently used substances. Ann ICRP. 2015;44:7–321.
Langen KJ, Bartenstein P, Boecker H, Brust P, Coenen HH, Drzezga A, et al. German guidelines for brain tumour imaging by PET and SPECT using labelled amino acids. Nuklearmedizin. 2011;50:167–73.
Acknowledgments
These guidelines were brought to the attention of all other EANM committees and the national societies of nuclear medicine, and received confirmatory statements from Italy, Latvia and Germany. The comments and suggestions from the EANM Radiation Protection and the Technologist Committee are highly appreciated and were considered in the preparation of these guidelines. We acknowledge the contribution of previous guidelines on which the present are based [10, 12, 13, 96].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The following authors declare that they have no conflicts of interest: Nathalie L Albert, Norbert Galldiks, Karl-Josef Langen, Egesta Lopci, Bernhard Sattler, Michael Weller.
Ian Law has received a speaker honorarium from Siemens Healthcare; Javier Arbizu has received research grants from Lilly-Avid, General Electric Healthcare and Piramal, and speaker honoraria from Biogen, Araclon Biotech-Grifols, Bayer and Novartis; Ronald Boellaard has received research grants from Philips Healthcare, Siemens Healthcare, BMS and Roche, and speaker honoraria from Philips Healthcare and Siemens Healthcare; Alexander Drzezga has received research grants from Siemens Healthcare and Lilly-Avid, and a speaker honorarium from Siemens Healthcare, owns stock in Siemens Healthcare, and is a member of an advisory committee for GE Healthcare; Christian la Fougère has received research grants from GE Healthcare and a speaker honorarium from GE Healthcare; Val Lowe has been a consultant for Bayer Schering Pharma, Piramal Life Sciences and Merck Research, and has received research support from GE Healthcare, Siemens Molecular Imaging and AVID Radiopharmaceuticals; Jonathan McConathy has received research support and has been a consultant for Blue Earth Diagnostic; Harald H. Quick has received research grants from Siemens Healthcare; David M. Schuster has received research grants from Blue Earth Diagnostics, Nihon MediPhysics Co. Ltd. and Advanced Accelerator Applications, and is a consultant for Syncona and American Imaging Management; Jörg-Christian Tonn has received research grants and a speaker honorarium from BrainLab, and owns stock in Johnson and Johnson.
Ethical approval
These guidelines do not describe any studies with human participants or animals performed by any of the authors.
Approval
These practice guidelines were approved by the Board of Directors of the EANM, SNMMI, EANO and PET RANO.
Additional information
The authors are members of the working group with the chair as first author followed by all the other members listed in alphabetical order by last name.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Law, I., Albert, N.L., Arbizu, J. et al. Joint EANM/EANO/RANO practice guidelines/SNMMI procedure standards for imaging of gliomas using PET with radiolabelled amino acids and [18F]FDG: version 1.0. Eur J Nucl Med Mol Imaging 46, 540–557 (2019). https://doi.org/10.1007/s00259-018-4207-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-4207-9