Abstract
The purpose of this study was to examine the volume and the composition of atherosclerotic plaque in symptomatic carotid arteries and to investigate the relationship between these plaque features and the severity of stenosis and the presence of cardiovascular risk factors. One hundred patients with cerebrovascular symptoms underwent CT angiography. We measured plaque volume (PV) and the relative contribution of plaque components (calcifications, fibrous tissue, and lipid) in the symptomatic artery. The contribution of different components was measured as the number of voxels within defined ranges of HU values (calcification >130 HU, fibrous tissue 60–130 HU, lipid core <60 HU). Fifty-seven patients had atherosclerotic plaque in the symptomatic carotid artery. The severity of stenosis and PV were moderately correlated. Age and smoking were independently related to PV. Patients with hypercholesterolemia had significantly less lipid and more calcium in their plaques than patients without hypercholesterolemia. Other cardiovascular risk factors were not significantly related to PV or plaque composition. Luminal stenosis of the carotid artery partly reflects the amount of atherosclerotic carotid disease. Plaque volume and plaque composition are associated with cardiovascular risk factors.
Similar content being viewed by others
Introduction
The causes of cerebral ischemia are multiple, but the three most common pathophysiological mechanisms are atherosclerotic large-vessel disease, intracranial small-vessel disease, and cardiac embolism. The severity of stenosis caused by atherosclerosis in the carotid bifurcation is an important risk factor for (recurrent) stroke and is used to decide which patients could benefit from carotid intervention, such as endarterectomy or stent placement [1]. However, luminal stenosis as a parameter of carotid artery disease does not necessarily reflect the amount of atherosclerosis. For example, most symptomatic patients have only mildly stenotic lesions [2]. This demonstrates that other plaque features play a role in an acute ischemic event.
Accumulation of atherosclerotic plaque in the carotid artery may lead to positive remodelling in which the artery enlarges to preserve the luminal area [3]. In addition, a certain amount of atherosclerosis should be present in the carotid bulb before it causes stenosis. Consequently, plaque volume is usually underestimated by the degree of stenosis. Rupture of an atherosclerotic plaque, which leads to embolization of thrombus or plaque material to the intracranial arteries, is considered an important underlying event of cerebrovascular symptoms. It is current opinion that plaque vulnerability to rupture is related to the composition of the plaque [4]. Therefore, plaque volume (PV) and plaque composition may be parameters that help in a better risk prediction and selection of patients who could benefit from surgical or endovascular intervention.
CT angiography has established itself as an accurate modality to assess the presence of atherosclerotic disease and to grade the severity of stenosis [5]. In addition, multidetector CT angiography (MDCTA) has the ability to identify and quantify different plaque components (lipid, fibrous tissue, and calcifications) [6–9].
In this cross-sectional study, we analyzed PV and the composition of atherosclerotic plaque in symptomatic carotid arteries with MDCTA to investigate the relationship between these plaque features and the severity of stenosis and the presence of cardiovascular risk factors. We hypothesized that (1) the severity of stenosis was not closely related to PV and (2) cardiovascular risk factors were more related to PV than to severity of stenosis.
Methods
Patients
We studied 100 consecutive patients with ischemic cerebrovascular symptoms in the territory of a nonoccluded carotid artery. The study was approved by the Institutional Review Board; all patients gave written informed consent.
CT protocol and image reconstruction
CT of the carotid arteries was performed on a 16-slice MDCT system (Siemens, Sensation 16, Erlangen, Germany) with a standardized optimized contrast-enhanced protocol (120 kVp, 180 mAs, collimation 16 × 0.75 mm, table feed 12 mm/rotation, pitch 1) [10].
Image reconstructions were made with a 120-mm field of view, a matrix size of 512 × 512, a slice thickness of 1.0 mm, an increment of 0.6 mm, and an intermediate reconstruction algorithm.
Volume of plaque and its components
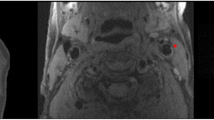
We measured plaque and plaque-component volumes with a polymeasure plug-in [9] for the freely available software package ImageJ (Rasband, National Institute of Mental Health, Bethesda, MD, USA) (Fig. 1).
Semi-automatic assessment of plaque component areas in MDCT images. Axial MDCT image of an atherosclerotic carotid plaque; the region of interest is drawn on the outer vessel wall (a). Ranges of Hounsfield units (HU) represent three different plaque components: yellow lipid core (<60 HU), red fibrous tissue (60–130 HU), and white calcification (>130 HU) (b)
This plug-in made it possible to draw ROIs over the outer vessel wall contour in consecutive axial MDCTA images and to automatically calculate the total number of pixels and the number of pixels of different Hounsfield unit (HU) ranges within these ROI. Different HU ranges represent different plaque components (Fig. 1).
The cut-off point between calcifications and fibrous tissue was set at 130 HU. The cut-off point between fibrous tissue and lipid was set at 60 HU as assessed in previous studies [6]. We adjusted the cut-off point between atherosclerotic plaque and lumen for each patient on the basis of the full width–half maximum principle [mean lumen attenuation plus mean fibrous tissue attenuation (≈88 HU) divided by two]. The pixels around the lumen, with a range between 130 HU and the adjusted cut-off value, were considered to be fibrous tissue.
To assess the border between lumen and atherosclerotic plaque, it was necessary to draw a second ROI in each image. Normally, the lumen area was then automatically differentiated from atherosclerotic plaque on the basis of the adjusted cut-off value. But in those plaques in which calcifications bordered the lumen and the two structures merged with each other, lumen area and calcifications had to be separated by manual drawing.
The volume of the atherosclerotic plaque and its components was calculated by multiplying the calculated number of pixels, the pixel size, and the increment. The proportion of plaque components was calculated as the ratio of volume of the component to the total plaque volume multiplied by 100. The length of the plaque was calculated by multiplying the number of slices that contained plaque by the increment (0.6 mm). Two observers (S.R, T.T.d.W.), who were blinded to other clinical information, performed the volume measurements in consensus.
In a previous study, we evaluated the reproducibility of the volume measurements in 56 symptomatic carotid arteries. The averaged interclass correlation coefficient was 0.88 for PV, 0.97 for percent calcification, 0.90 for percent fibrous tissue, and 0.76 for percent lipid tissue [9].
Severity of stenosis
One observer (C.d.M.) measured the severity of stenosis according to the NASCET criteria on MPR images parallel to the central lumen line. If juxtaluminal calcifications were present, the window setting was widened to prevent overestimation of the luminal stenosis.
We divided the severity of stenosis into five categories (0, 1–29, 30–49, 50–69, and 70–99%).
Cardiovascular risk factors
We obtained clinical measures and information on risk factors and medication during the patient’s visit at the outpatient clinic. Subjects were categorized as currently, ever, or never smoking. Hypertension was defined as systolic blood pressure over 140 and/or diastolic blood pressure over 90 mmHg during two episodes of at least 15 min of continuous noninvasive blood-pressure measurement and/or treatment with antihypertensive medication. Blood pressure-lowering drugs comprised ACE inhibitors, calcium-antagonists, beta-blockers, and diuretics.
Hypercholesterolemia was defined as fasting cholesterol over 5.0 mmol/l and/or use of cholesterol-lowering drugs. Diabetes was defined as fasting serum glucose levels over 7.9 mmol/l, nonfasting serum glucose levels over 11.0 mmol/l, or use of antidiabetic medication.
Information was collected on previous cardiovascular events and conditions (myocardial infarction, atrial fibrillation, angina pectoris, chronic heart failure, coronary artery bypass grafting) and previous cerebrovascular events.
Statistical analysis
Data are presented as mean ± SD. Spearman’s correlation coefficients (Rs) were calculated to analyze the relations between (1) severity of stenosis and PV, (2) the proportion of plaque components and PV, and (3) age and PV.
Because the distribution of plaque volume and severity of stenosis were skewed, we used logistic regression to determine the associations between cardiovascular risk factors and PV or stenosis. The highest quartile of volume or stenosis was compared to the lower three quartiles. Firstly, age and gender were entered into the model. Secondly, all cardiovascular risk factors were added. To analyze the association of cardiovascular risk factors with plaque composition, we used linear regression, adjusting for age, sex, PV, and all risk factors. Because the distribution of the proportion of plaque components was skewed, we made a natural log-transformation (ln). To calculate the mean ln proportion of plaque components for the presence of significant cardiovascular risk factors, we used analysis of covariance (ANCOVA), adjusting for age, sex, PV, and all other risk factors. Because severe calcification may hamper the quantification of lipid [6], we repeated the analyses in which the contribution of plaque components was involved, after exclusion of severely calcified plaques (defined as >20% calcifications). SPSS 11.0 for Windows (SPSS, Chicago, IL, USA) was used for data analysis.
Results
Baseline characteristics
The baseline clinical characteristics are presented in Table 1. Fifty-seven of 100 patients had atherosclerotic plaque in the symptomatic carotid artery. The length of the 57 symptomatic atherosclerotic plaques was 20.9 ± 13.5 mm (range 3.6–70.2 mm). PV of the 57 atherosclerotic plaques was 773 ± 685 mm3. Fibrous tissue and lipid were present in all plaques. Calcifications were present in 54 of the 57 plaques. The contribution of the lipid, fibrous, and calcified plaque components was 18 ± 12, 68 ± 14, and 13 ± 11%, respectively. Thirty-five of the 54 patients (65%) with minor stroke, 9 of the 19 patients (47%) with transient ischemic attack (TIA), and 13 of the 27 patients (48%) with amaurosis fugax (AF) had atherosclerotic plaque in their symptomatic artery. The PV in patients with minor stroke (884 ± 627 mm3) was larger than the PV in patients with TIA (783 ± 957 mm3; P = 0.19) and the PV in patients with AF (469 ± 573 mm3; P < 0.01) The contribution of calcifications was larger in minor stroke patients than in AF patients (15 ± 12% versus 9 ± 6; P < 0.05).
Plaque volume and severity of stenosis
Table 2 shows the volume of the plaque and the contribution of the plaque components for the different grades of stenosis. In 20 out of 61 patients with a stenosis grade of 0%, atherosclerotic plaque was present (PV = 411 ± 472 mm3). In 18 of the 20 patients with a stenosis grade of 1–29%, plaque was present with a PV of 543 ± 464 mm3. The correlation between PV and severity of stenosis in the group of patients who had an atherosclerotic plaque (n = 57) was moderate with an Rs of 0.66 (P < 0.0001) (Figs. 2 and 3).
CT angiograms of the carotid bifurcation with lesion. Sagittal (a, d) and axial (b, c, e, f) images of atherosclerotic plaques in the carotid bifurcation. The left panels show an extensive calcified atherosclerotic plaque [plaque volume (PV) = 1,318 mm3] without severe stenosis (20%). The right panels reveal a focal lesion at the origin of the internal carotid artery with a moderate amount of atherosclerosis (PV = 169 mm3) but severe stenosis (73%)
Plaque volume and plaque composition
Figure 4 shows the relationship between the contribution of calcium, fibrous tissue, and lipid, and total PV in the 57 patients with atherosclerotic plaque. With increasing PV, the contribution of fibrous tissue decreased (Rs = -0.83, P < 0.001) and the contribution of lipid increased (Rs = 0.62, P < 0.001). With an increase in PV, the contribution of calcium increased slightly (Rs = 0.42, P = 0.001). After exclusion of severely calcified plaques, we still revealed an increase in the contribution of lipid with increasing PV (Rs = 0.64, P = 0.001).
Scatter plot demonstrates the relation between the contribution of the three different plaque components and total plaque volume in 57 patients. The gray line represents the contribution of lipid, the dotted line represents the contribution of fibrous tissue, and the solid black line represents the contribution of calcifications to the total plaque volume
Risk factors
There was a moderate relationship between age and PV for both men and women (Rs = 0.493, P = 0.001 and Rs = 0.484, P < 0.001, respectively). Table 3 shows the age and gender-adjusted odds ratios (ORs) and 95% confidence intervals (95% CI) and the multivariable adjusted ORs and 95% CIs for associations between cardiovascular risk factors and (1) atherosclerotic carotid PV and (2) severity of stenosis (upper quartile versus lower three quartiles). Smoking was independently related to PV (OR 4.9, 95% CI 1.2–19.3) and to severity of stenosis (OR 4.6, 95% CI 1.2–18.1).
Subsequently, we analyzed the association between plaque composition and cardiovascular risk factors. Patients with hypercholesterolemia had a significantly higher contribution of calcium and a significantly lower contribution of lipid in the atherosclerotic plaque. The mean proportion of calcium in the plaque of patients with and without hypercholesterolemia was 9.9 and 2.0%, respectively. The ln mean difference was 1.61 (95% CI 0.70–2.53). The mean proportion of lipid in the plaque of patients with and without hypercholesterolemia was 12.2 and 26.0%, respectively. The ln mean difference was -0.76 (95% CI -1.14 to -0.38). After exclusion of severely calcified plaques, patients with hypercholesterolemia again showed a significantly lower contribution of lipid in the atherosclerotic plaque than patients without hypercholesterolemia (2.2 and 20.2%, respectively).
Discussion
In this study, we quantified and characterized atherosclerotic carotid plaque with MDCTA and examined whether the relation between PV and the severity of luminal stenosis was strong. A moderate association between the severity of luminal stenosis and PV was described in the present study. Smoking was associated with both PV and severity of stenosis. Our hypothesis that cardiovascular risk factors were more strongly associated with PV than severity of stenosis was not supported in this study. We demonstrated that an increasing PV is associated with a change in plaque composition: the proportion of calcium and lipid increases and the proportion of fibrous tissue decreases. Finally, hypercholesterolemia was independently related to plaque composition.
Plaque volume and stenosis
There are several reasons why severity of stenosis is not a good reflection of the amount of atherosclerotic disease. Firstly, extensive atherosclerotic disease can be present without stenosis of the lumen, and vice versa, stenosis can be caused by a focal accumulation of a small amount of atherosclerotic plaque (Fig. 3). Secondly, the configuration of a normal carotid bulbus and bifurcation allows the accumulation of extensive atherosclerotic plaque before a luminal stenosis becomes visible on angiography. Thirdly, vessel remodelling plays an additional role since the discrepancy between the atherosclerotic plaque load and angiographic appearance of the lumen is also present in other vessel beds. A recent MRI study showed that luminal stenosis provides an incomplete picture of atherosclerotic progression and regression and that expansive remodelling occurs specifically in the earlier stage of atherosclerosis development in carotid arteries [11].
It is well known that atherosclerosis with low-grade stenosis in the carotid bifurcation may result in cerebrovascular events [12]. In the present study, a relatively large proportion of the patients with cerebrovascular symptoms had atherosclerotic plaque with no luminal narrowing measured according to the NASCET criteria. Since PV is a better descriptor of the severity of atherosclerotic disease than degree of stenosis, and CT and MRI now allow the quantification of atherosclerotic plaque, we advocate evaluating the role of PV as an additional parameter in the assessment of stroke risk and ultimately in treatment decision-making.
Plaque volume and composition
The composition of the atherosclerotic plaque changes during the progression of atherosclerotic disease, and this plays an important role in the development of a vulnerable plaque. Until now, most data on the temporal change in the composition of the atherosclerotic plaque have been based on cross-sectional studies in which vessel specimens obtained during autopsy or operation (carotid endarterectomy) were evaluated. Atherosclerotic plaques were classified based on their composition and that classification was considered to reflect the temporal natural history of atherosclerotic disease [13]. Such studies have provided tremendous information on the process of atherosclerotic disease and the occurrence of clinical events. However, much more can be expected from serial evaluation of an atherosclerotic plaque with clinical imaging tools because this will truly provide insight into the natural history of atherosclerotic plaque and into the causal association of changes in plaque composition and clinical events. With regard to the natural history, the present cross-sectional imaging study shows that plaque composition changes with increasing PV. According to the AHA criteria, which describe advanced atherosclerotic lesions in the carotid artery as containing more lipid and more calcium, we found an increase in the proportions of lipid and calcification with increasing PV. It will be of interest to confirm these temporal changes in PV and composition with serial MDCTA.
Plaque volume and cardiovascular risk factors
The relation between cardiovascular risk factors and the severity of atherosclerotic disease is difficult to evaluate, and most studies have correlated cardiovascular risk factors with indirect instead of direct measures of atherosclerotic plaque burden [14]. Several large population-based studies have demonstrated independent associations between cardiovascular risk factors such as smoking, hypertension, hypercholesterolemia, and diabetes and ultrasound (US)-measured intima-media thickness (IMT) in the carotid artery [15], severity of stenosis in the carotid artery [16], carotid calcification [17], coronary stenosis [14], and coronary calcification [14].
In our study, smoking was independently related to severity of stenosis and PV. Other risk factors did not reach a statistically significant association due to the limited number of studied patients. Severity of stenosis as an indirect parameter of atherosclerotic plaque burden has its limitations. It reflects luminal narrowing and not the true amount of atherosclerotic disease. Two recent studies demonstrated that the relation between severity of stenosis and cardiovascular risk factors was less strong than the relation between intravascular US-assessed atherosclerotic plaque burden and cardiovascular risk factors [18, 19]. Nicholls et al. concluded that different mechanisms probably drive stenosis development and atheroma accumulation [18].
Plaque composition and cardiovascular risk factors
Plaque composition is considered an important feature of the so-called vulnerable plaque. Histological studies that examined carotid endarterectomy specimens have shown that the composition of the plaque is influenced by cardiovascular risk factors: hypercholesterolemia and hyperfibrinogenemia were correlated with plaques rich in foam cells [20, 21].
To our knowledge, this is the first study that describes the relationship between the proportions of three different carotid plaque components measured with MDCTA and risk factors for atherosclerosis. We found that hypercholesterolemia was independently associated with the proportion of lipid and calcium in the plaque. In comparison to the histological studies, we found that patients with hypercholesterolemia had a smaller proportion of lipid and a larger proportion of calcium in their symptomatic plaques. This might be explained by the large proportion of patients on lipid-lowering drugs. IVUS studies in coronary arteries have revealed that statins reduce the lipid content of atherosclerotic plaques [22]. MRI studies on the carotid plaque have shown that prolonged lipid-lowering drug therapy is associated with markedly decreased lipid content [23].
Limitations
The first limitation of this study is the relatively small number of patients on whom we performed our analysis. We expect that analysis of a larger number of patients will provide more evidence for the associations we investigated. A second limitation is the cross-sectional design of this study. Longitudinal studies are necessary to prove the value of PV as a parameter for risk stratification. A third limitation concerns the validation of CT to accurately distinguish plaque components. Until now, CT and histology have been compared side by side to define the range of HU values for the different tissue types. Validation of these cut-off points in a new prospective sample of patients is required. A fourth limitation concerns the identification of hemorrhage and thrombus. Wintermark et al. reported that they could assess large intraplaque haemorrhage, defined with the range of 72–177 Hounsfield units, with a kappa of 0.712 between CTA and histology [8]. However, we were not able to confirm this in our own validation study and have therefore restricted our analysis to calcifications, fibrous tissue, and lipid core.
Despite these limitations, the conclusion of our study might have some clinical implications. Firstly, the quantity of atherosclerotic plaque, expressed as plaque volume, was moderately associated with the severity of stenosis, which implies that PV might be an important additional parameter in the analysis of atherosclerosis in the carotid artery. Secondly, PV and plaque composition are related to each other and to risk factors for atherosclerosis. Noninvasive imaging of these plaque parameters will increase the understanding of the natural history of atherosclerotic disease in humans.
References
Anonymous (1991) Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 325:445–453
Dahl T, Cederin B, Myhre HO, Indredavik B (2008) The prevalence of carotid artery stenosis in an unselected hospitalized stroke population. Int Angiol 27:142–145
Glagov S, Weisenberg E, Zarins CK, Stankunavicius R, Kolettis GJ (1987) Compensatory enlargement of human atherosclerotic coronary arteries. N Engl J Med 316:1371–1375
Naghavi M, Libby P, Falk E, Casscells SW, Litovsky S, Rumberger J, Badimon JJ, Stefanadis C, Moreno P, Pasterkamp G, Fayad Z, Stone PH, Waxman S, Raggi P, Madjid M, Zarrabi A, Burke A, Yuan C, Fitzgerald PJ, Siscovick DS, de Korte CL, Aikawa M, Juhani Airaksinen KE, Assmann G, Becker CR, Chesebro JH, Farb A, Galis ZS, Jackson C, Jang IK, Koenig W, Lodder RA, March K, Demirovic J, Navab M, Priori SG, Rekhter MD, Bahr R, Grundy SM, Mehran R, Colombo A, Boerwinkle E, Ballantyne C, Insull W Jr, Schwartz RS, Vogel R, Serruys PW, Hansson GK, Faxon DP, Kaul S, Drexler H, Greenland P, Muller JE, Virmani R, Ridker PM, Zipes DP, Shah PK, Willerson JT (2003) From vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: part I. Circulation 108:1664–1672
Koelemay MJ, Nederkoorn PJ, Reitsma JB, Majoie CB (2004) Systematic review of computed tomographic angiography for assessment of carotid artery disease. Stroke 35:2306–2312
de Weert TT, Ouhlous M, Meijering E, Zondervan PE, Hendriks JM, van Sambeek MR, Dippel DW, van der Lugt A (2006) In vivo characterization and quantification of atherosclerotic carotid plaque components with multidetector computed tomography and histopathological correlation. Arterioscler Thromb Vasc Biol 26:2366–2372
Nandalur KR, Hardie AD, Raghavan P, Schipper MJ, Baskurt E, Kramer CM (2007) Composition of the stable carotid plaque: insights from a multidetector computed tomography study of plaque volume. Stroke 38:935–940
Wintermark M, Jawadi SS, Rapp JH, Tihan T, Tong E, Glidden DV, Abedin S, Schaeffer S, Acevedo-Bolton G, Boudignon B, Orwoll B, Pan X, Saloner D (2008) High-resolution CT imaging of carotid artery atherosclerotic plaques. AJNR Am J Neuroradiol 29:875–882
de Weert TT, de Monye C, Meijering E, Booij R, Niessen WJ, Dippel DW, van der Lugt A (2008) Assessment of atherosclerotic carotid plaque volume with multidetector computed tomography angiography. Int J Cardiovasc Imaging 24:751–759
de Monye C, Cademartiri F, de Weert TT, Siepman DA, Dippel DW, van der Lugt A (2005) Sixteen-detector row CT angiography of carotid arteries: comparison of different volumes of contrast material with and without a bolus chaser. Radiology 237:555–562
Saam T, Yuan C, Chu B, Takaya N, Underhill H, Cai J, Tran N, Polissar NL, Neradilek B, Jarvik GP, Isaac C, Garden GA, Maravilla KR, Hashimoto B, Hatsukami TS (2007) Predictors of carotid atherosclerotic plaque progression as measured by noninvasive magnetic resonance imaging. Atherosclerosis 194(2):e34–42
Wasserman BA, Wityk RJ, Trout HH 3rd, Virmani R (2005) Low-grade carotid stenosis: looking beyond the lumen with MRI. Stroke 36:2504–2513
Stary HC, Chandler AB, Dinsmore RE, Fuster V, Glagov S, Insull W Jr, Rosenfeld ME, Schwartz CJ, Wagner WD, Wissler RW (1995) A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Arterioscler Thromb Vasc Biol 15:1512–1531
Schmermund A, Baumgart D, Gorge G, Gronemeyer D, Seibel R, Bailey KR, Rumberger JA, Paar D, Erbel R (1998) Measuring the effect of risk factors on coronary atherosclerosis: coronary calcium score versus angiographic disease severity. J Am Coll Cardiol 31:1267–1273
Bots ML, Hofman A, De Jong PT, Grobbee DE (1996) Common carotid intima-media thickness as an indicator of atherosclerosis at other sites of the carotid artery. The Rotterdam Study. Ann Epidemiol 6:147–153
Mast H, Thompson JL, Lin IF, Hofmeister C, Hartmann A, Marx P, Mohr JP, Sacco RL (1998) Cigarette smoking as a determinant of high-grade carotid artery stenosis in Hispanic, black, and white patients with stroke or transient ischemic attack. Stroke 29:908–912
Allison MA, Criqui MH, Wright CM (2004) Patterns and risk factors for systemic calcified atherosclerosis. Arterioscler Thromb Vasc Biol 24:331–336
Nicholls SJ, Tuzcu EM, Crowe T, Sipahi I, Schoenhagen P, Kapadia S, Hazen SL, Wun CC, Norton M, Ntanios F, Nissen SE (2006) Relationship between cardiovascular risk factors and atherosclerotic disease burden measured by intravascular ultrasound. J Am Coll Cardiol 47:1967–1975
Kahlon JP, Torey J, Nordstrom CK, LaLonde TA, Ali A, Schreiber TL, Ogawa T, Maciejko JJ, Rosman H, Gardin JM (2006) The impact of coronary artery disease risk factors on intravascular ultrasound-derived morphologic indices of human coronaries. Echocardiography 23:308–311
Spagnoli LG, Mauriello A, Palmieri G, Santeusanio G, Amante A, Taurino M (1994) Relationships between risk factors and morphological patterns of human carotid atherosclerotic plaques. A multivariate discriminant analysis. Atherosclerosis 108:39–60
Mauriello A, Sangiorgi G, Palmieri G, Virmani R, Holmes DR Jr, Schwartz RS, Pistolese R, Ippoliti A, Spagnoli LG (2000) Hyperfibrinogenemia is associated with specific histocytological composition and complications of atherosclerotic carotid plaques in patients affected by transient ischemic attacks. Circulation 101:744–750
Kawasaki M, Sano K, Okubo M, Yokoyama H, Ito Y, Murata I, Tsuchiya K, Minatoguchi S, Zhou X, Fujita H, Fujiwara H (2005) Volumetric quantitative analysis of tissue characteristics of coronary plaques after statin therapy using three-dimensional integrated backscatter intravascular ultrasound. J Am Coll Cardiol 45:1946–1953
Zhao XQ, Yuan C, Hatsukami TS, Frechette EH, Kang XJ, Maravilla KR, Brown BG (2001) Effects of prolonged intensive lipid-lowering therapy on the characteristics of carotid atherosclerotic plaques in vivo by MRI: a case-control study. Arterioscler Thromb Vasc Biol 21:1623–1629
Acknowledgements
Aad van der Lugt is recipient of a fellowship from the Netherlands Organisation for Scientific Research (NWO-KF grant no. 907-00-122).
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Rozie, S., de Weert, T.T., de Monyé, C. et al. Atherosclerotic plaque volume and composition in symptomatic carotid arteries assessed with multidetector CT angiography; relationship with severity of stenosis and cardiovascular risk factors. Eur Radiol 19, 2294–2301 (2009). https://doi.org/10.1007/s00330-009-1394-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-009-1394-6