Abstract
Objectives
To compare the contrast agent effect of a full dose and half the dose of gadobenate dimeglumine in brain tumours at 7 Tesla (7T) MR versus 3 Tesla (3T).
Methods
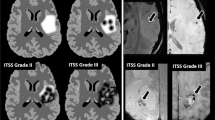
Ten patients with primary brain tumours or metastases were examined. Signal intensities were assessed in the lesion and normal brain. Tumour-to-brain contrast and lesion enhancement were calculated. Additionally, two independent readers subjectively graded the image quality and artefacts.
Results
The enhanced mean tumour-to-brain contrast and lesion enhancement were significantly higher at 7T than at 3T for both half the dose (91.8 ± 45.8 vs. 43.9 ± 25.3 [p = 0.010], 128.1 ± 53.7 vs. 75.5 ± 32.4 [p = 0.004]) and the full dose (129.2 ± 50.9 vs. 66.6 ± 33.1 [p = 0.002], 165.4 ± 54.2 vs. 102.6 ± 45.4 [p = 0.004]). Differences between dosages at each field strength were also significant. Lesion enhancement was higher with half the dose at 7T than with the full dose at 3T (p = .037), while the tumour-to-brain contrast was not significantly different. Subjectively, contrast enhancement, visibility, and lesion delineation were better at 7T and with the full dose. All parameters were rated as good, at the least.
Conclusion
Half the routine contrast agent dose at 7T provided higher lesion enhancement than the full dose at 3T which indicates the possibility of dose reduction at 7T.
Key Points
• The contrast effect of gadobenate dimeglumine was assessed at 7T and 3T.
• In brain tumours, contrast effect was higher at 7T than at 3T.
• Tumour-to-brain contrast at 7T half dose and 3T full dose were comparable.
• 7T half dose lesion enhancement was higher than 3T full dose enhancement.
• Our results indicate the possibility of contrast agent dose reduction at 7T.




Similar content being viewed by others
References
Brem SS, Bierman PJ, Brem H et al (2011) Central nervous system cancers. J Natl Compr Cancer Netw 9:352–400
Haustein J, Laniado M, Niendorf HP et al (1992) Administration of gadopentetate dimeglumine in MR imaging of intracranial tumors - dosage and field-strength. Am J Neuroradiol 13:1199–1206
Moser E, Stahlberg F, Ladd ME et al (2012) 7-T MR-from research to clinical applications? NMR Biomed 25:695–716
Yuh WTC, Fisher DJ, Runge VM et al (1994) Phase-III multicenter trial of high-dose gadoteridol in MR evaluation of brain metastases. Am J Neuroradiol 15:1037–1051
Akeson P, Vikhoff B, Stahlberg F et al (1997) Brain lesion contrast in MR imaging - dependence on field strength and concentration of gadodiamide injection in patients and phantoms. Acta Radiol 38:14–18
Chang KH, Ra DG, Han MH et al (1994) Contrast enhancement of brain-tumors at different MR field strengths - comparison of 0.5-T and 2.0-T. Am J Neuroradiol 15:1413–1419
Krautmacher C, Willinek WA, Tschampa HJ et al (2005) Brain tumors: full- and half-dose contrast-enhanced MR imaging at 3.0T compared with 1.5T - initial experience. Radiology 237:1014–1019
Nobauer-Huhmann IM, Ba-Ssalamah A, Mlynarik V et al (2002) Magnetic resonance imaging contrast enhancement of brain tumors at 3 tesla versus 1.5 tesla. Investig Radiol 37:114–119
Griswold MA, Jakob PM, Heidemann RM et al (2002) Generalized autocalibrating partially parallel acquisitions (GRAPPA). Magn Reson Med 47:1202–1210
Runge VM, Biswas J, Wintersperger BJ et al (2006) The efficacy of gadobenate dimeglumine (Gd-BOPTA) at 3 tesla in brain magnetic resonance imaging - comparison to 1.5 tesla and a standard gadolinium chelate using a rat brain tumor model. Investig Radiol 41:244–248
Rinck PA, Fischer HW, Vanderelst L et al (1988) Field-cycling relaxometry - medical applications. Radiology 168:843–849
Wansapura JP, Holland SK, Dunn RS et al (1999) NMR relaxation times in the human brain at 3.0 tesla. JMRI-J Magn Reson Imaging 9:531–538
Wood ML, Hardy PA (1993) Proton relaxation enhancement. JMRI-J Magn Reson Imaging 3:149–156
Fernandez-Seara MA, Wehrli FW (2000) Postprocessing technique to correct for background gradients in image-based R-2(*) measurements. Magn Reson Med 44:358–366
Vogler H, Platzek J, SchuhmannGiampieri G et al (1995) Pre-clinical evaluation of gadobutrol: a new, neutral, extracellular contrast agent for magnetic resonance imaging. Eur J Radiol 21:1–10
Rohrer M, Bauer H, Mintorovitch J et al (2005) Comparison of magnetic properties of MRI contrast media solutions at different magnetic field strengths. Investig Radiol 40:715–724
Pintaske J, Martirosian P, Graf H et al (2006) Relaxivity of gadopentetate dimeglumine (Magnevist), gadobutrol (Giadovist), and gadobenate dimeglumine (MultiHance) in human blood plasma at 0.2, 1.5, and 3 Tesla. Investig Radiol 41:213–221
Noebauer-Huhmann IM, Szomolanyi P, Juras V et al (2010) Gadolinium-based magnetic resonance contrast agents at 7 tesla in vitro T-1 relaxivities in human blood plasma. Investig Radiol 45:554–558
Rinck PA, Muller RN (1999) Field strength and dose dependence of contrast enhancement by gadolinium-based MR contrast agents. Eur Radiol 9:998–1004
Sze G, Johnson C, Kawamura Y et al (1998) Comparison of single- and triple-dose contrast material in the MR screening of brain metastases. Am J Neuroradiol 19:821–828
Schneider G, Kirchin MA, Pirovano G et al (2001) Gadobenate dimeglumine-enhanced magnetic resonance imaging of intracranial metastases: effect of dose on lesion detection and delineation. J Magn Reson Imaging 14:525–539
Ba-Ssalamah A, Nobauer-Huhmann IM, Pinker K et al (2003) Effect of contrast dose and field strength in the magnetic resonance detection of brain metastases. Investig Radiol 38:415–422
Runge VM, Kirsch JE, Burke VJ et al (1992) High-dose gadoteridol in MR imaging of intracranial neoplasms. JMRI-J Magn Reson Imaging 2:9–18
Brekenfeld C, Foert E, Hundt W et al (2001) Enhancement of cerebral diseases: how much contrast agent is enough? Comparison of 0.1, 0.2, and 0.3 mmol/kg gadoteridol at 0.2T with 0.1 mmol/kg gadoteridol at 1.5T. Investig Radiol 36:266–275
Bracco (2012) Prescribing information. Bracco Diagnostics Inc
Schorner W, Laniado M, Niendorf HP et al (1986) Time-dependent changes in image-contrast in brain-tumors after gadolinium-DTPA. Am J Neuroradiol 7:1013–1020
Runge VM, Gelblum DY, Pacetti ML et al (1990) Gd-Hp-Do3a in clinical MR imaging of the brain. Radiology 177:393–400
Liang JC, Sammet S, Yang XY et al (2010) Intraindividual in vivo comparison of gadolinium contrast agents for pharmacokinetic analysis using dynamic contrast enhanced magnetic resonance imaging. Investig Radiol 45:233–244
Kuhn MJ, Picozzi P, Maldjian JA et al (2007) Evaluation of intraaxial enhancing brain tumors on magnetic resonance imaging: intraindividual crossover comparison of gadobenate dimeglumine and gadopentetate dimeglumine for visualization and assessment, and implications for surgical intervention. J Neurosurg 106:557–566
Rumboldt Z, Rowley HA, Steinberg F et al (2009) Multicenter, double-blind, randomized, intra-individual crossover comparison of gadobenate dimeglumine and gadopentetate dimeglumine in MRI of brain tumors at 3 Tesla. J Magn Reson Imaging 29:760–767
Acknowledgements
The scientific guarantor of this publication is Prof. Christian Herold, M.D. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. Funding support provided by the Austrian Science Fund (FWF) P 25246 B24, Vienna Advanced Imaging Center (VIACLIC) des Wiener Wissenschafts-und Technologie Fonds (WWTF) FA102A0017, and the Slovak Scientific Grant Agency VEGA (VEGA2/0013/14). One of the authors has significant statistical expertise.
Institutional Review Board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. Study subjects or cohorts have not been previously reported. Methodology: prospective, experimental, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Noebauer-Huhmann, IM., Szomolanyi, P., Kronnerwetter, C. et al. Brain tumours at 7T MRI compared to 3T—contrast effect after half and full standard contrast agent dose: initial results. Eur Radiol 25, 106–112 (2015). https://doi.org/10.1007/s00330-014-3351-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3351-2