Abstract
Objective
To predict sensorineural hearing loss (SNHL) and neurological impairment in congenital cytomegalovirus (cCMV) infection using MR imaging and define the best timing in pregnancy for prenatal assessment.
Methods
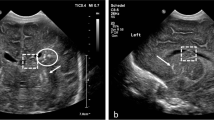
In 121 patients with confirmed cCMV infection, brain features at MR imaging were respectively graded from 1 to 5: normal; isolated frontal/parieto–occipital hyperintensity; temporal periventricular hyperintensity; temporal/occipital cysts and/or intraventricular septa; migration disorders. Grading was correlated with postnatal SNHL and neurological impairment using regression analysis. In 51 fetuses with MR examinations at 26.9 and 33.0 weeks, the predictive value of SNHL and neurological impairment was compared using ROC curves.
Results
Postnatal follow-up showed SNHL in 18 infants and neurological impairment in 10. MR grading was predictive of SNHL and of neurological impairment (P < 0.001). In grade 1 or 2, none had SNHL and 1/74 had neurological impairment. The areas under ROC curves for prediction of postnatal SNHL and of neurological impairment from first and second MR examination were comparable.
Conclusion
Our data suggest that in cCMV infection, prediction of SNHL and neurological impairment is feasible by fetal MR imaging with a high negative predictive value and can equally be done at 27 or 33 weeks of gestation.
Key points
• In cCMV, isolated periventricular T2-weighted signal hyperintensity has a good postnatal prognosis.
• In cCMV, SNHL and neurological impairment can be predicted at 27 or 33 weeks.
• In cCMV, fetal MR has a high NPV in predicting SNHL.
• In cCMV, fetal MR has a high NPV in predicting neurological impairment.




Similar content being viewed by others
References
Kenneson A, Cannon MJ (2007) Review and meta-analysis of the epidemiology of congenital cytomegalovirus (CMV) infection. Rev Med Virol 17:253–276
Stagno S, Pass RF, Cloud G et al (1986) Primary cytomegalovirus infection in pregnancy. Incidence, transmission to fetus, and clinical outcome. JAMA 256:1904–1908
Nance WE, Lim BG, Dodson KM (2006) Importance of congenital cytomegalovirus infections as a cause for pre-lingual hearing loss. J Clin Virol 35:221–225
Iwasaki S, Yamashita M, Maeda M, Misawa K, Mineta H (2007) Audiological outcome of infants with congenital cytomegalovirus infection in a prospective study. Audiol Neurootol 12:31–36
Pass RF, Fowler KB, Boppana SB, Britt WJ, Stagno S (2006) Congenital cytomegalovirus infection following first trimester maternal infection: symptoms at birth and outcome. J Clin Virol 35:216–220
Foulon I, Naessens A, Foulon W, Casteels A, Gordts F (2008) Hearing loss in children with congenital cytomegalovirus infection in relation to the maternal trimester in which the maternal primary infection occurred. Pediatrics 122:e1123–e1127
Enders G, Daiminger A, Bäder U, Exler S, Enders M (2011) Intrauterine transmission and clinical outcome of 248 pregnancies with primary cytomegalovirus infection in relation to gestational age. J Clin Virol 52:244–246
Lipitz S, Yinon Y, Malinger G et al (2013) Risk of cytomegalovirus-associated sequelae in relation to time of infection and findings on prenatal imaging. Ultrasound Obstet Gynecol 41:508–514
Benoist G, Salomon LJ, Mohlo M, Suarez B, Jacquemard F, Ville Y (2008) Cytomegalovirus-related fetal brain lesions: comparison between targeted ultrasound examination and magnetic resonance imaging. Ultrasound Obstet Gynecol 32:900–905
Picone O, Simon I, Benachi A, Brunelle F, Sonigo P (2008) Comparison between ultrasound and magnetic resonance imaging in assessment of fetal cytomegalovirus infection. Prenat Diagn 28:753–758
Lipitz S, Hoffmann C, Feldman B, Tepperberg-Dikawa M, Schiff E, Weisz B (2010) Value of prenatal ultrasound and magnetic resonance imaging in assessment of congenital primary cytomegalovirus infection. Ultrasound Obstet Gynecol 36:709–717
Doneda C, Parazzini C, Righini A et al (2010) Early cerebral lesions in cytomegalovirus infection: prenatal MR imaging. Radiology 255:613–621
van der Knaap MS, Vermeulen G, Barkhof F, Hart AA, Loeber JG, Weel JF (2004) Pattern of white matter abnormalities at MR imaging: use of polymerase chain reaction testing of Guthrie cards to link pattern with congenital cytomegalovirus infection. Radiology 230:529–536
Tilea B, Alberti C, Adamsbaum C et al (2009) Cerebral biometry in fetal magnetic resonance imaging: new reference data. Ultrasound Obstet Gynecol 33:173–181
Parazzini C, Righini A, Rustico M, Consonni D, Triulzi F (2008) Prenatal magnetic resonance imaging: brain normal linear biometric values below 24 gestational weeks. Neuroradiology 50:877–883
Bayley N (2006) Screening Test of Bayley Scales of Infant and Toddler Development-III. San Antonio, Pearson
Brandt I (2001) Griffiths Entwicklungsskalen (GES) zur Beurteilung der Entwicklung in den ersten beiden Lebensjahren. Hogrefe-Verlag
Snijders JT, Snijders-Oomen N (1976) Snijders-Oomen non-verbal intelligence scale, S.O.N. 21/ –7. HD 2 Tjeenk Willink, Groningen
Wechsler D (2002) WPPSI-III administration and scoring manual. Psychological Corporation, San Antonio
Wechsler D (2002) WPPSI-III technical and interpretive manual. Psychological Corporation, San Antonio
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Widmalm SE, Brooks SL, Sano T, Upton LG, McKay DC (2006) Limitation of the diagnostic value of MR images for diagnosing temporomandibular joint disorders. Dentomaxillofac Radiol 35:334–338
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143:29–36
Hanley JA, McNeil BJ (1983) A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 148:839–843
Foulon I, Naessens A, Faron G, Foulon W, Jansen AC, Gordts F (2012) Hearing thresholds in children with a congenital CMV infection: a prospective study. Int J Pediatr Otorhinolaryngol 76:712–717
Yoshinaga-Itano C, Sedey AL, Coulter DK, Mehl AL (1998) Language of early- and later-identified children with hearing loss. Pediatrics 102:1161–1171
Bernal B, Perdomo J. Brodmann’s Interactive Atlas 1.1. http://www.fmriconsulting.com/brodmann/
Cheeran MC, Lokensgard JR, Schleiss MR (2009) Neuropathogenesis of congenital cytomegalovirus infection: disease mechanisms and prospects for intervention. Clin Microbiol Rev 22:99–126
Marques Dias MJ, Harmant-van Rijckevorsel G, Landrieu P, Lyon G (1984) Prenatal cytomegalovirus disease and cerebral microgyria: evidence for perfusion failure, not disturbance of histogenesis, as the major cause of fetal cytomegalovirus encephalopathy. Neuropediatrics 15:18–24
Jacquemard F, Yamamoto M, Costa JM et al (2007) Maternal administration of valaciclovir in symptomatic intrauterine cytomegalovirus infection. BJOG 114:1113–1121
Ville Y. In utero treatment of cytomegalovirus congenital infection with valacyclovir (CYMEVAL). NIH-Clinical trials 2012. http://clinicaltrials.gov/ct2/show/NCT01651585?term=Cytomegalovirus++congenital&recr=Open&rank=8
Spong CY, Thom E. A randomized trial to prevent congenital cytomegalovirus (CMV). NIH Clinical trials 2012. http://clinicaltrials.gov/ct2/show/NCT01376778?term=Cytomegalovirus++congenital&recr=Open&rank=3
Walker SP, Palma-Dias R, Wood EM, Shekleton P, Giles ML (2013) Cytomegalovirus in pregnancy: to screen or not to screen. BMC Pregnancy Childbirth 13:96
Foulon I, Naessens A, Foulon W, Casteels A, Gordts F (2008) A 10-year prospective study of sensorineural hearing loss in children with congenital cytomegalovirus infection. J Pediatr 153:84–88
Lanari M, Lazzarotto T, Venturi V et al (2006) Neonatal cytomegalovirus blood load and risk of sequelae in symptomatic and asymptomatic congenitally infected newborns. Pediatrics 117:e76–e83
Acknowledgments
The scientific guarantor of this publication is Prof Jacques Jani. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. This study has received funding by the Fetal Medicine Foundation Belgium. Lei Ding kindly provided statistical advice for this manuscript. Institutional review board approval was obtained. Written informed consent was waived by the Institutional Review Board.
Some study subjects or cohorts have been previously reported in: Foulon I, Naessens A, Foulon W, Casteels A, Gordts F (2008) Hearing loss in children with congenital cytomegalovirus infection in relation to the maternal trimester in which the maternal primary infection occurred. Pediatrics 122:e1123-1127 and Foulon I, Naessens A, Faron G, Foulon W, Jansen AC, Gordts F (2012) Hearing thresholds in children with a congenital CMV infection: a prospective study. Int J Pediatr Otorhinolaryngol 76:712-717. Methodology: retrospective, prognostic study/observational, multicentre study.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 18 kb)
Rights and permissions
About this article
Cite this article
Cannie, M.M., Devlieger, R., Leyder, M. et al. Congenital cytomegalovirus infection: contribution and best timing of prenatal MR imaging. Eur Radiol 26, 3760–3769 (2016). https://doi.org/10.1007/s00330-015-4187-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-4187-0