Abstract
Background
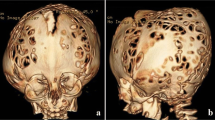
Syndromic craniosynostoses (Saethre–Chotzen, Pfeiffer 1, 2, 3, Apert, Crouzon, mainly) are particular in this that a single gene defect (mostly fibroblast growth factor receptor [FGFR] 2) generates different clinical phenotypes that characterize these syndromes. Significant brain abnormalities have been reported in all syndromes. However, whether these abnormalities are secondary to the bone disease or primary (e.g. callosal agenesis) is still controversial. Recent evidence suggests that the white matter defect might be a primary disorder.
Review of literature
From the review of the literature and the analysis of our cases, it appears that three categories of brain abnormalities can be found. (1) The global distortion of the brain is likely mechanical and in keeping with the deformity of the skull. (2) The chronic tonsillar herniation (Chiari I deformity) is likely mechanical also and a consequence of the small size of the posterior fossa, especially after an early closure (before 24 m) of the lambdoid suture. (3) On the contrary, the constellation of abnormalities that selectively involve the white matter (non-progressive, non-destructive ventriculomegaly, callosal agenesis or thinning, agenesis of septum pellucidum, paucity of the antero-mesial temporal white matter, pyramidal hypoplasia) is much more likely to constitute a primary disorder.
Conclusions
Recent neurobiological evidence supports this point of view. L1 cell adhesion molecule (L1CAM) gene plays a major role in the development of the white matter and its mutation in humans (callosal agenesis, retardation, adducted thumbs, spasticity, and hydrocephalus syndrome, Bickers–Adams syndrome) or in mice causes similar defects of the corpus callosum, septum pellucidum, centrum semi-ovale, and cortico-spinal tracts. To operate, L1CAM need interactions with FGFRs, whose defects are causal to the syndromic craniosynostoses. It seems logical to assumes that the FGFR defects generate both the skull abnormalities and, by lack of interaction with L1CAM, the primary defect of the white matter. The mental deficiency that is common in these patients therefore is likely to be part of the disease (through the L1CAM–FGFR interaction) rather than a consequence of the skull size or of the associated hydrocephalus.









Similar content being viewed by others
References
ten Donkelaar HJ, Lammens M, Hori A (2006) Clinical neuroembryology. Development and developmental disorders of the human central nervous system. Springer, Berlin
Jones KL (2006) Smith’s recognizable pattern of human malformation, 6th edn. Elsevier Saunders, Philadelphia, PA
OMIM (2007) Online Mendelian inheritance in man. Johns Hopkins University, Baltimore, MD
Carinci F, Pezzetti F, Becchetti E, Carls F, Avantaggiato A, Becchetti A, Carinci P, Baroni T, Bodo M (2005) Apert and Crouzon syndromes: clinical findings, genes and extracellular matrix. J Craniofac Surg 16:361–368
Da Costa AC, Walters I, Savarirayan R, Anderson VA, Wrennall JA, Meara JG (2006) Intellectual outcomes in children and adolescent with syndromic and nonsyndromic craniosynostosis. Plast Reconstr Surg 118:182–183
Elia M, Musumeci SA, Ferri R, Greco D, Romano C, Del Gracco S, Stefanini MC (1996) Saethre-Chotzen syndrome: a clinical, EEG and neuroradiological study. Child’s Nerv Syst 12:699–704
Gabrielli O, Moroni E, Barbato M, Pierleoni C, Felici L (1989) Acrocefalosindatillia tipo III (S. Saethre–Chotzen). Descrizione di due casi. Pathologia 81:295–300 (quoted by [6])
Philip N, Chabrol B, Lossi AM, Cardoso C, Guerrini R, Dobyns WB, Raybaud C, Villard L (2003) Mutations in the oligophrenin-1 gene (OPHN1) cause X-linked congenital cerebellar hypoplasia. J Med Genet 40:441–446
Cohen MM Jr (1993) Pfeiffer syndrome update, clinical subtypes, and guidelines for differential diagnosis. Am J Med Genet 45:300–307
Robin NH, Scott JA, Arnold JE, Goldstein JA, Shilling BB, Marion RW, Cohen MM Jr (1998) Favorable prognosis for children with Pfeiffer syndrome types 2 and 3: implication for classification. Am J Med Genet 75:240–244
Plomp AS, Hamel BCJ, Cobben JM, Verloes A, Offermans JPM, Lajeunie E, Fryns JP, de Die-Smulders CEM (1998) Pfeiffer syndrome type 2: further delineation and review of the literature. Am J Med Genet 75:245–51
Barkovich AJ (2005) Pediatric neuroimaging, 4th edn. Lippincott Williams & Wilkins, Philadelphia
Colosimo C, Tartaro A, Cama A, Tortori-Donati P (2005) The craniosynostoses. In: Tortori-Donati P, Rossi A, Biancheri R (eds) Pediatric neuroradiology. Springer, Berlin, pp 1289–1315
Itoh S, Nojima M, Yoshida K (2006) Usefulness of magnetic resonance imaging for accurate diagnosis of Pfeiffer syndrome type II in utero. Fetal Diagn Ther 21:168–171
Fjortoft MI, Sevely A, Boetto S, Kessler S, Sarramon F, Rolland M (2007) Prenatal diagnosis of craniosynostosis: value of MR imaging. Neuroradiology 49:515–521
Francis PM, Beals S, Rekate HL, Pittman HW, Manwaring K, Reiff J (1992) Chronic tonsillar herniation and Crouzon’s syndrome. Pediatr Neurosurg 18:202–206
Tokumaru AM, Barkovich AJ, Ciricillo SF, Edwards MSB (1996) Skull base and calvarial deformities: association with intracranial changes in craniofacial syndromes. Am J Neuroradiol 17:619–630
Cohen MM Jr, Kreiborg S, Lammer EJ, Cordero JF, Mastroiacovo P, Erickson JD, Roeper P, Martinez-Frias ML (1992) Birth prevalence study of the Apert syndrome. Am J Med Genet 42:655–659
Lajeunie E, Cameron R, El Ghouzi V, de Parseval N, Journeau P, Gonzales M, Delezoide AL, Bonaventure J, Le Merrer M, Renier D (1999) Clinical variability in patients with Apert’s syndrome. J Neurosurg 90:443–447
Patton MA, Goodship J, Hayward R, Lansdown R (1988) Intellectual development in Apert’s syndrome: a long term follow-up of 29 patients. J Med Genet 25:164–167
Maksem JA, Roessmann U (1979) Apert’s syndrome with central nervous system anomalies. Acta Neuropathol 48:59–61
De Leon GA, de Leon G, Grover WD, Zaeri N, Alburger PD (1987) Agenesis of the corpus callosum and limbic malformation in Apert syndrome (type I acrocephalosyndactyly). Arch Neurol 44:979–982
Cohen MM Jr, Kreiborg S (1990) The central nervous system in the Apert syndrome. Am J Med Genet 35:36–45
Cohen MM Jr, Kreiborg S (1993) An updated pediatric perspective on the Apert syndrome. Am J Dis Child 147:989–993
Yacubian-Fernandes A, Palhares A, Giglio A, Gabarra RC, Zanini S, Portela L, Plese JPP (2004) Apert syndrome: analysis of associated brain malformations and conformational changes determined by surgical treatment. J Neuroradiol 31:116–122
Quitero-Rivera F, Robson CD, Reiss RE, Levine D, Benson CB, Mulliken JB, Kimonis VE (2006) Intracranial anomalies detected by imaging studies in 30 patients with Apert syndrome. Am J Med Genet Part A 140A:1337–1338
Renier D, Arnaud E, Cinalli G, Sebag G, Zerah M, Marchac D (1996) Prognosis for mental function in Apert’s syndrome. J Neurosurg 85:66–72
Yacubian-Fernandes A, Palhares A, Giglio A, Gabarra RC, Zanini S, Portela L, Silva MV, Perosa GB, Abramides D, Plese JPP (2005) Apert syndrome: factors involved in the cognitive development. Arq Neuropsiquiatr 63:963–968
Cinalli G, Renier D, Sebag G, Sainte-Rose C, Arnaud E, Pierre-Kahn A (1995) Chronic tonsillar herniation in Crouzon and Apert’s syndromes: the role of premature synostosis of the lambdoid suture. J Neurosurg 83:575–582
Raybaud C, Girard N (2005) Malformations of the telencephalic commissures. In: Tortori-Donati P, Rossi A, Biancheri R (eds) Pediatric neuroradiology. Springer, Berlin, pp 41–69
Shu T, Shen WB, Richards LJ (2001) Development of the perforating pathway: an ipsilateral pathway between the medial septum/diagonal band of Broca and the cingulate cortex that intersects the corpus callosum. J Comp Neurol 436:411–422
ten Donkelaar HJ, Lammens M, Wesseling P, Hori A, Keyser A, Roteveel J (2004) Development and malformations of the human pyramidal tract. J Neurol 251:1429–1442
Hoefkens M, Vermeij-Keers C, Vaandrager JM (2004) Crouzon syndrome phenotypic signs and symptoms of the postnatally expressed subtype. J Craniofac Surg 15:233–242
Proudman TW, Clark BE, Moore MH, Abbott AH, David DJ (1995) Central nervous system imaging in Crouzon’s syndrome. J Craniofac Surg 6:401–405
Taravath S, Tonsgard JH (1993) Cerebral malformation in Carpenter syndrome. Pediat Neurol 9:230–234
Demyanenko GP, Tsay AY, Maness PF (1999) Abnormalities in neuronal process extension, hippocampal development and the ventricular system of L1 knockout mice. J Neurosci 19:4907–4920
Finckh U, Schröder J, Ressler B, Veske A, Gal A (2000) Spectrum of detection rate of L1CAM mutations in isolated and familial cases with suspected L1-disease. Am J Med Genet 92:40–46
Kamiguchi H, Lemmon V (1997) Neural cell adhesion molecule L1: signaling pathways and growth cone motility. J Neurosc Res 49:1–8
Doherty P, Walsh F (1996) CAM-FGF receptor interactions: a model for axonal growth. Mol Cell Neurosci 8:99–111
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Raybaud, C., Di Rocco, C. Brain malformation in syndromic craniosynostoses, a primary disorder of white matter: a review. Childs Nerv Syst 23, 1379–1388 (2007). https://doi.org/10.1007/s00381-007-0474-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-007-0474-7