Abstract
Background
We report two cases of diffuse cerebellar swelling with upward transtentorial herniation following medulloblastoma resection. We present our insight for managing medulloblastoma with aggressive clinical behavior.
Review summary
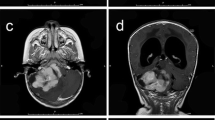
Case 1 is a 32-month-old boy. Magnetic resonance imaging (MRI) revealed fourth ventricular mass with diffuse leptomeningeal metastasis. He underwent gross total resectioning of the tumor and histopathology revealed a large cell medulloblastoma. A ventriculoperitoneal shunt was placed on the 25th postoperative day. Ten days after he developed lethargy, and MRI showed diffuse cerebellar swelling with upward herniation. He underwent emergent posterior fossa decompression; however, he remained unresponsive since then. Case 2 is a 31-month-old boy. MRI revealed a fourth ventricular mass with diffuse leptomeningeal metastasis. He underwent gross total resection and histopathology was a large cell medulloblastoma. Due to developing ventriculomegaly, extraventricular drainage was reinserted on the 11th postoperative day. Four days after, he developed lethargy and decerebrate posturing. MRI showed diffuse cerebellar swelling with upward herniation. He underwent aggressive posterior fossa decompression. Chemotherapy was started postoperatively. Gradually, his movement of extremities improved. On the 79th postoperative day, he started to follow commands and talk some words. He was discharged to a rehabilitation institute and has continued to improve since then.
Conclusion
Diffuse cerebellar swelling with upward herniation could occur in patients with aggressive medulloblastoma postoperatively. Our patients had diffuse leptomeningeal dissemination of the tumor at the initial presentation. Close monitoring and prompt diagnosis with earlier surgical posterior fossa decompression and administration of chemotherapy may prevent irreversible neurologic deterioration.





Similar content being viewed by others
References
Brown HG, Kepner JL, Perlman EJ et al (2000) “Large cell/anaplastic” medulloblastomas: a Pediatric Oncology Group Study. J Neuropathol Exp Neurol 59:857–865
Davis FG, Freels S, Grutsch J, Barlas S, Brem S (1998) Survival rates in patients with primary brain tumors stratified by patient age and tumor histological type: an analysis based on Surveillance, Epidemiology and End Results (SEER) data, 1973–1991. J Neurosurg 88:1–10
David KF, Casey ATH, Hayward RD, Harkness WFJ, Phipps K, Wade AM (1997) Medulloblastoma: is the 5-year survival rate improving?—A review of 80 cases from a single institution. J Neurosurg 86:13–21
Gajjar A, Chintagumpala M, Ashley D et al (2006) Risk-adapted craniospinal radiotherapy followed by high-dose chemotherapy and stem-cell rescue in children with newly diagnosed medulloblastoma (St. Jude Medulloblastoma-96): long-term results from a prospective, multicentre trial. Lancet Oncol 10:813–820
Ishihara H, Kubota H, Lindberg RL et al (2008) Endothelial cell barrier impairment induced by glioblastomas and transforming growth factor beta2 involves matrix metalloproteinases and tight junction proteins. J Neuropathol Exp Neurol 67:435–448
Papadopoulos MC, Saadoun S, Binder DK, Manley GT, Krishna S, Verkman AS (2004) Molecular mechanisms of brain tumor edema. Neuroscience 129:1011–1020
Strugar J, Rothbart D, Harrington W, Criscuolo GR (1994) Vascular permeability factor in brain metastases: correlation with vasogenic brain edema and tumor angiogenesis. J Neurosurg 81:560–566
Taylor RE, Bailey CC, Robinson KJ et al (2005) Outcome of patients with metastatic (M2-3) medulloblastoma treated with SIOP/UKCCSG PNET III chemotherapy. Eur J Cancer 41:727–734
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ogiwara, H., Dipatri, A.J., Bowman, R.M. et al. Diffuse postoperative cerebellar swelling in medulloblastoma: report of two cases. Childs Nerv Syst 27, 743–747 (2011). https://doi.org/10.1007/s00381-010-1343-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-010-1343-3