Abstract
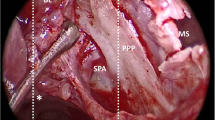
Intractable posterior epistaxis (PE) is a frequent emergency for which different treatment modalities are available. While nasal packing causes extreme discomfort and angiography with consecutive selective embolization is not available everywhere, recent studies emphasize the value of sphenopalatine artery (SPA) occlusion by different techniques and indicate success rates of 13–33%. In our institution, previously endoscopic management of PE consisted either of isolated coagulation of an identified bleeding source (group A) or cutting and coagulation of arterial branches running through the sphenopalatine foramen (SPF) (group B). According to our neuroradiological and rhinological experience we developed a modification of SPA transsection and coagulation following identification of the division in conchal and septal branches of the SPA (group C). During a 26-month period the success rates of these three techniques in 95 patients were compared prospectively. The three modalities revealed a re-bleeding rate of 3 out of 21 (21%) in group A, 1 in 6 (16.7%) in group B and 3 in 69 (4.3%) in group C. At the level of the SPF, 36 out of 69 patients had one conchal branch, whereas 30 (43.5%) had two and 3 (4.4%) had three. If SPA transsection and coagulation for intractable PE is adopted the anatomic varieties of the SPA with its division in conchal and septal branches have to be taken into account. According to our experience the septal branch of the SPA plays a major role in PE. Its occlusion significantly improves the success rate of PE treatment.

Similar content being viewed by others
References
Balrow DW, Deleyiannis WB, Pinczower EF (1997) Effectiveness of surgical management of epistaxis at a tertiary care center. Laryngoscope 107: 21–24
Breda SD, Choi IS, Persky MS, Weiss M (1989) Embolization in the treatment of epistaxis after failure of internal maxillary artery ligation. Laryngoscope 99: 809–813
Budrovich M, Saetti R (1992) Microscopic and endoscopic ligature of the sphenopalatine artery. Laryngoscope 102: 1390–1394
Chandler JR, Serrins AJ (1965) Transantral ligation of the internal maxillary artery of epistaxis. Laryngoscope 75: 1151–1159
Elden L, Montanera W, TerBrugge K, Willinsky R, Lasjaunias P, Chalres D (1994) Angiographic embolization for the treatment of epistaxis: a review of 108 cases. Otolaryngol Head Neck Surg 111: 44–50
Lang J (1988). Klinische Anatomie der Nase, Nasenhöhle und Nasennebenhöhlen. Georg Thieme Verlag, Stuttgart, New York, pp 102–105
Lasjaunias P, Vignaud J, Hasso AN (1975) Maxillary artery blood supply to the orbit: normal and pathological aspects. Neuroradiology 9: 87–97
Mc Donald TJ, Pearson PW (1980) Follow-up on maxillary artery ligation for epistaxis. Arch Otolaryngol 106: 635–638
Merland JJ, Melki JP, Chiras J (1982) Place of embolization in the treatment of severe epistaxis. J Otolaryngol 11: 271–274
Metson R, Hanson DG (1983) Bilateral facial nerve paralysis following arterial embolization for epistaxis. Otolaryngol Head Neck Surg 91: 299–303
Montgomery WW, Reardon EJ (1980) Early vessel ligation for control of severe epistaxis. In: Snow JB Jr (ed) Controversies in otolaryngology. WB Saunders, Philadelphia, pp 315–319
O'Flynn PE, Shadaba A (2000) Management of posterior epistaxis by endoscoic clipping of the sphenopalatine artery. Clin Otolaryngol 25: 374–377
Parnes LS, Heeneman H, Vinuela F (1987) Percutaneous embolization for control of nasal blood circulation. Laryngoscope 97: 1312–1315
Prades J (1976) Abord endonasal de la fosse pterygo-maxillaire. LXXIII Cong Franc Compt Rendus des Seance: 290–296
Rockey JG, Anand R (2002) A critical audit of the surgical management of intractable epistaxis using sphenopalatine artery ligation/diathermy. Rhinology 40: 147–149
Snyderman CH, Goldman SA, Carrau RL, Ferguson BJ Grandis JR (1999) Endoscopic sphenopalatine artery ligation is an effective method of treatment for posterior epistaxis. Am J Rhinol 13: 137–140
Sokoloff J, Wickbom I, McDonald D (1974) Therapeutic percutaneous embolization in intractable epistaxis. Radiology 111: 285–287
Strutz J Schumacher M (1990) Uncontrollable epistaxis. Arch Otolaryngol Head Neck Surg 116: 697–699
Valavanis A, Setton A (1993) Embolization of epistaxis. In: Valavanis A (ed) Interventional neuroradiolergy. Spinger, Berlin, Heidelberg, New York, pp 55–61
Vitek JJ (1991) Idiopathic intractable epistaxis: endovascular therapy. Radiology 181: 113–116
Voegels RL, Thomé DC, Iturralde PPV, Butugan OB (2001) Endoscopic ligature of the sphenopalatine artery for severe posterior epistaxis. Otolaryngol Head Neck Surg 124: 464–467
Weaver EM, Chaloupka JC, Putman CM, Roth TC, Horky JK, Sasaki CT (1999) Effect of internal maxillary arterial occlusion on nasal blood flow in swine. Laryngoscope 109: 8–14
Welsh LW, Welsh JJ, Scogna JE, Gregor FA (1990) Role of angiography in the management of refractory epistaxis. Ann Otol Rhinol Laryngol 99: 69–73
Author information
Authors and Affiliations
Corresponding author
Additional information
For this study, neither financial support nor funding was given.
Rights and permissions
About this article
Cite this article
Holzmann, D., Kaufmann, T., Pedrini, P. et al. Posterior epistaxis: endonasal exposure and occlusion of the branches of the sphenopalatine artery. Eur Arch Otorhinolaryngol 260, 425–428 (2003). https://doi.org/10.1007/s00405-003-0618-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-003-0618-7