Abstract
Background and purpose
Although gait disturbance is an important feature of idiopathic normal pressure hydrocephalus (NPH), only tentative theories have been offered to explain its pathophysiology. It has been suggested that the mesencephalic locomotor region is the anatomical substrate for the development of the hypokinetic NPH gait. To investigate this possibility, we evaluated the correlation between gait disturbance and midbrain diameter.
Methods
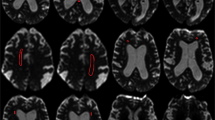
We enrolled 21 patients with NPH and 20 age–matched control subjects for the study. The maximal diameter of the midbrain and pons, and the width of the lateral and third ventricles were measured using midsagittal T1–weighted MRI and axial T2–weighted MRI, respectively. Gait disturbance, cognitive dysfunction, and incontinence were semiquantified.
Results
The maximal midbrain diameter was significantly smaller in the NPH group than in the controls (14.8 ± 0.9 vs. 17.1 ± 0.7mm, p < 0.001). There were inverse correlations between the midbrain diameter and the widths of the two ventricles (r = –0.562, p = 0.008 for the third ventricle, and r = –0.510, p = 0.018 for the lateral ventricle). The severity of gait disturbance was negatively correlated with the midbrain diameter (r = –0.598, p = 0.004), but the degree of cognitive dysfunction and incontinence showed no significant correlation with midbrain diameter or ventricular width.
Conclusions
This study suggests that midbrain atrophy is significantly associated with gait disturbance in NPH.
Similar content being viewed by others
References
Achiron A, Ziv I, Goren M, Goldberg H, Zoldan Y, Sroka H, Melamed E (1993) Primary progressive freezing gait. Mov Disord 8:293–297
Adams RD, Fisher CM, Hakim S, Ojemann RG, Sweet WH (1965) Symptomatic occult hydrocephalus with ‘normal’ cerebrospinal fluid pressure. A treatable syndrome. N Engl J Med 273:117–126
Curran T, Lang AE (1994) Parkinsonian syndromes associated with hydrocephalus: case reports, a review of the literature, and pathophysiological hypotheses. Mov Disord 9:508–520
Ebersbach G, Sojer M, Valldeoriola F, Wissel J, Muller J, Tolosa E, Poewe W (1999) Comparative analysis of gait in Parkinson’s disease, cerebellar ataxia and subcortical arteriosclerotic encephalopathy. Brain 122:1349–1355
Fisher CM (1982) Hydrocephalus as a cause of disturbances of gait in the elderly. Neurology 32:1358–1363
Gai WP, Halliday GM, Blumbergs PC, Geffen LB, Blessing WW (1991) Substance P-containing neurons in the mesopontine tegmentum are severely affected in Parkinson’s disease. Brain 114:2253–2267
Garcia-Rill E (1991) The pedunculopontine nucleus (Review). Prog Neurobiol 36:363–389
Geula C, Schatz CR, Mesulam MM (1993) Differential localization of NADPH-diaphorase and calbindin- D28k within the cholinergic neurons in the basal forebrain, striatum and brainstem in the rat,monkey, baboon and human. Neuroscience 54:461–476
Graff-Radford NR, Godersky JC (1986) Normal pressure hydrocephalus. Onset of gait abnormality before dementia predicts good surgical outcome. Arch Neurol 43:940–942
Hakim S, Adams RD (1965) The special clinical problem of symptomatic hydrocephalus with normal cerebrospinal fluid pressure.Observations on cerebrospinal fluid hydrodynamics. J Neurol Sci 2:307–327
Inglis WL, Winn P (1995) The pedunculopontine tegmental nucleus: where the striatum meets the reticular formation. Prog Neurobiol 47:1–29
Ishii N, Nishihara Y, Imamura T (1986) Why do frontal lobe symptoms predominate in vascular dementia with lacunes? Neurology 36:340–345
Jankovic J, Newmark M, Peter P (1986) Parkinsonism and acquired hydrocephalus. Mov Disord 1:59–64
Jankovic J, Nutt JG, Sudarsky L (2001) Classification, diagnosis, and etiology of gait disorders. Adv Neurol 87:119–133
Jellinger K (1988) The pedunculopontine nucleus in Parkinson’s disease, progressive supranuclear palsy and Alzheimer’s disease. J Neurol Neurosurg Psychiatry 51:540–543
Juncos JL, Hirsch EC, Malessa S, Duyckaerts C, Hersh LB, Agid Y (1991) Mesencephalic cholinergic nuclei in progressive supranuclear palsy. Neurology 41:25–30
Knutsson E, Lying-Tunell U (1985) Gait apraxia in normal-pressure hydrocephalus: patterns of movement and muscle activation. Neurology 35:155–160
Krauss JK, Droste DW (1994) Predictability of intracranial pressure oscillations in patients with suspected normal pressure hydrocephalus by transcranial Doppler ultrasound. Neurol Res 16:398–402
Krauss JK, Faist M, Schubert M, Borremans JJ, Lucking CH, Berger W (2001) Evaluation of gait in normal pressure hydrocephalus before and after shunting. Adv Neurol 87:301–310
Krauss JK, Regel JP, Vach W, Jungling FD, Droste DW, Wakhloo AK (1997) Flow void of cerebrospinal fluid in idiopathic normal pressure hydrocephalus of the elderly: can it predict outcome after shunting? Neurosurgery 40:67–73
Larsson A, Moonen M, Bergh AC, Lindberg S, Wikkelso C (1990) Predictive value of quantitative cisternography in normal pressure hydrocephalus. Acta Neurol Scand 81:327–332
Larsson A, Wikkelso C, Bilting M, Stephensen H (1991) Clinical parameters in 74 consecutive patients shunt operated for normal pressure hydrocephalus. Acta Neurol Scand 84:475–482
Lee MS, Rinne JO, Marsden CD (2000) The pedunculopontine nucleus: its role in the genesis of movement disorders. Yonsei Med J 41:167–184
Malm J, Kristensen B, Fagerlund M, Koskinen LO, Ekstedt J (1995) Cerebrospinal fluid shunt dynamics in patients with idiopathic adult hydrocephalus syndrome. J Neurol Neurosurg Psychiatry 58:715–723
Masdeu JC (2001) Central disequilibrium syndromes. Adv Neurol 87:183–189
Masdeu JC, Alampur U, Cavaliere R, Tavoulareas G (1994) Astasia and gait failure with damage of the pontomesencephalic locomotor region. Ann Neurol 35:619–621
Miwa S, Inagaki C, Fujiwara M, Takaori S (1982) The activities of noradrenergic and dopaminergic neuron systems in experimental hydrocephalus. J Neurosurg 57:67–73
Nutt JG, Marsden CD, Thompson PD (1993) Human walking and higherlevel gait disorders, particularly in the elderly (comments). Neurology 43:268–279
Owler BK, Momjian S, Czosnyka Z, Czosnyka M, Pena A, Harris NG, Smielewski P, Fryer T, Donovan T, Coles J, Carpenter A, Pickard JD (2004) Normal pressure hydrocephalus and cerebral blood flow: a PET study of baseline values. J Cereb Blood Flow Metab 24:17–23
Pahapill PA, Lozano AM (2000) The pedunculopontine nucleus and Parkinson’s disease. Brain 123:1767–1783
Soelberg Sorensen P, Jansen EC, Gjerris F (1986) Motor disturbances in normal-pressure hydrocephalus. Special reference to stance and gait. Arch Neurol 43:34–38
Stolze H, Kuhtz-Buschbeck JP, Drucke H, Johnk K, Diercks C, Palmie S, Mehdorn HM, Illert M, Deuschl G (2000) Gait analysis in idiopathic normal pressure hydrocephalus–which parameters respond to the CSF tap test? Clin Neurophysiol 111:1678–1686
Stolze H, Kuhtz-Buschbeck JP, Drucke H, Johnk K, Illert M, Deuschl G (2001) Comparative analysis of the gait disorder of normal pressure hydrocephalus and Parkinson’s disease. J Neurol Neurosurg Psychiatry 70:289–297
Sudarsky L, Simon S (1987) Gait disorder in late-life hydrocephalus. Arch Neurol 44:263–267
Tanaka A, Okuzumi H, Kobayashi I, Murai N, Meguro K, Nakamura T (1995) Gait disturbance of patients with vascular and Alzheimer-type dementias. Percept Mot Skills 80:735–738
Thompson PD (2001) Gait disorders accompanying diseases of the frontal lobes. Adv Neurol 87:235–241
Thompson PD, Marsden CD (1987) Gait disorder of subcortical arteriosclerotic encephalopathy: Binswanger’s disease. Mov Disord 2:1–8
Turner B, Ramli N, Blumhardt LD, Jaspan T (2001) Ventricular enlargement in multiple sclerosis: a comparison of three-dimensional and linear MRI estimates. Neuroradiology 43:608–614
Warmuth-Metz M, Naumann M, Csoti I, Solymosi L (2001) Measurement of the midbrain diameter on routine magnetic resonance imaging: a simple and accurate method of differentiating between Parkinson disease and progressive supranuclear palsy. Arch Neurol 58:1076–1079
Zeidler M, Dorman PJ, Ferguson IT, Bateman DE (1998) Parkinsonism associated with obstructive hydrocephalus due to idiopathic aqueductal stenosis. J Neurol Neurosurg Psychiatry 64:657–659
Zweig RM, Jankel WR,Hedreen JC, Mayeux R, Price DL (1989) The pedunculopontine nucleus in Parkinson’s disease. Ann Neurol 26:41–46
Zweig RM, Whitehouse PJ, Casanova MF, Walker LC, Jankel WR, Price DL (1987) Loss of pedunculopontine neurons in progressive supranuclear palsy. Ann Neurol 22:18–25
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, P.H., Yong, S.W., Ahn, Y.H. et al. Correlation of midbrain diameter and gait disturbance in patients with idiopathic normal pressure hydrocephalus. J Neurol 252, 958–963 (2005). https://doi.org/10.1007/s00415-005-0791-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-005-0791-2