Abstract
Background
The BENEFIT study examined interferon beta (IFNB)-1b treatment in patients with clinically isolated syndrome (CIS) and ≥ 2 clinically silent brain MRI lesions.
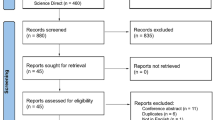
Methods
Subgroups of 468 patients (IFNB-1b: n = 292; placebo: n = 176) were created for demographics, clinical, laboratory, and MRI findings at onset. The 'natural' risk of clinically definite MS (CDMS) over 2 years was estimated by Kaplan Meier statistics in placebo-treated patients; the IFNB-1b treatment effect was analysed by Cox proportional hazards regression.
Results
The risk of CDMS was increased in placebotreated patients (overall 45 %) if they were younger (< 30 years: 60%), were cerebrospinal fluid (CSF)-positive (49 %), or had received steroid treatment (48 %). MRI parameters implied a higher risk in placebo-treated patients with ≥ 9 T2-lesions (48%) or ≥ 1 gadolinium (Gd)-enhancing lesions (52 %). The CDMS risk was highest (75 %) in placebo-treated patients with monofocal disease onset displaying MRI disease activity (≥ 1 Gd-lesion) and dissemination (≥ 9 T2-lesions). Treatment effects were significant across almost all subgroups including patients with less disease dissemination/activity at onset (monofocal: 55%; < 9 T2-lesions: 60%; no Gd-lesions: 57%) and patients without steroid treatment for the CIS (62 %). Monofocal patients had greater treatment effects if they had ≥ 9 T2-lesions (61 %), Gd-lesions (58 %), or both (65 %).
Conclusions
This study confirms the impact of age of onset, CSF and MRI findings on risk of conversion from CIS to CDMS. IFNB-1b treatment effect was robust across the study population including patients without MRI disease activity and less clinical or MRI disease dissemination at onset and patients not receiving steroids for the CIS.
Similar content being viewed by others
References
Barkhof F, Filippi M, Miller DH, et al. (1997) Comparison of MRI criteria at first presentation to predict conversion to clinically definite multiple sclerosis. Brain 120 (Pt 11):2059–2069
Barkhof F, Rocca M, Francis G, et al. (2003) Validation of diagnostic magnetic resonance imaging criteria for multiple sclerosis and response to interferon beta1a. Ann Neurol 53:718–724
Beck RW, Chandler DL, Cole SR, et al. (2002) Interferon beta-1a for early multiple sclerosis: CHAMPS trial subgroup analyses. Ann Neurol 51:481–90
Beck RW, Cleary PA, Anderson MM Jr, et al. (1992) A randomized, controlled trial of corticosteroids in the treatment of acute optic neuritis. The Optic Neuritis Study Group. N Engl J Med 326:581–588
CHAMPS Study Group (2002) Predictors of short-term disease activity following a first clinical demyelinating event: analysis of the CHAMPS placebo group. Mult Scler 8:405–409
Confavreux C, Vukusic S, Adeleine P (2003) Early clinical predictors and progression of irreversible disability in multiple sclerosis: an amnesic process. Brain 126:770–782
European Study Group on interferon beta-1b in secondary progressive MS (1998) Placebo-controlled multicentre randomised trial of interferon beta-1b in treatment of secondary progressive multiple sclerosis. Lancet 352:1491–1497
Held U, Heigenhauser L, Shang C, Kappos L, Polman C (2005) Predictors of relapse rate in MS clinical trials. Neurology 65:1769–1773
IFNB Multiple Sclerosis Study Group (1993) Interferon beta-1b is effective in relapsing-remitting multiple sclerosis. I. Clinical results of a multicenter, randomised, double-blind, placebo-controlled trial. Neurology 43:655–661
Jacobs LD, Beck RW, Simon JH, et al. (2000) Intramuscular interferon beta- 1a therapy initiated during a first demyelinating event in multiple sclerosis. CHAMPS Study Group. N Engl J Med 343:898–904
Kappos L, Polman CH, Freedman MS, et al. (2005) Treatment with interferon beta-1b delays conversion to clinically definite and McDonald MS in patients with clinically isolated syndromes. Neurology 67:1242–1249
Korteweg T, Tintore M, Uitdehaag B, et al. (2006) MRI criteria for dissemination in space in patients with clinically isolated syndromes: a multicentre follow-up study. Lancet Neurol 5:221–227
Li DK, Held U, Petkau J, et al. (2006) MRI T2 lesion burden in multiple sclerosis: a plateauing relationship with clinical disability. Neurology 66:1384–1389
Miller DH, Molyneux PD, Barker GJ, et al. (1999) Effect of interferon-beta1b on magnetic resonance imaging outcomes in secondary progressive multiple sclerosis: results of a European multicenter, randomized, doubleblind, placebo-controlled trial. Ann Neurol 46:850–859
O'Connor P (2003) The effects of intramuscular interferon beta-Ia in patients at high risk for development of multiple sclerosis: a post hoc analysis of data from CHAMPS. Clin Ther 25:2865–2874
Paty DW, Li DK (1993) Interferon beta-1b is effective in relapsing-remitting multiple sclerosis. II. MRI analysis results of a multicenter, randomized, double-blind, placebo-controlled trial. Neurology 43:662–667
Poser CM, Paty DW, Scheinberg L, et al. (1983) New diagnostic criteria for multiple sclerosis: guidelines for research protocols. Ann Neurol 13:227–231
Soderstrom M, Ya-Ping J, Hillert J, Link H (1998) Optic neuritis: prognosis for multiple sclerosis from MRI, CSF, and HLA findings. Neurology 50:708–714
Tintore M, Rovira A, Brieva L, et al. (2001) Isolated demyelinating syndromes: comparison of CSF oligoclonal bands and different MR imaging criteria to predict conversion to CDMS. Mult Scler 7:359–363
Tintore M, Rovira A, Rio J, et al. (2005) Is optic neuritis more benign than other first attacks in multiple sclerosis? Ann Neurol 57:210–215
Uitdehaag BM, Kappos L, Bauer L, et al. (2005) Discrepancies in the interpretation of clinical symptoms and signs in the diagnosis of multiple sclerosis. A proposal for standardization. Mult Scler 11:227–231
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Data analysis was performed by S. Dahms.
Disclosures
C. Polman has received: consulting fees from Biogen Idec, Bayer Schering Pharma AG, Teva, Serono, Novartis, Antisense, and GlaxoSmithKline; lecture fees from Biogen Idec, Bayer Schering Pharma AG, and Teva and grant support from Biogen Idec, Bayer Schering Pharma AG, Wyeth, and Glaxo-SmithKline.
L.Kappos has received honoraria and research support from the Swiss MS Society, Aventis, Bayer, Berlex, Biogen Idec, Elan, Genzyme, GlaxoSmithKline, Novartis, Bayer Schering Pharma AG, Serono, Teva, Wyeth, and others. These payments were exclusively used for support of MS research at his department.
M. Freedman has received honoraria from Serono, Bayer Schering Pharma AG, Berlex, Teva, Pfizer, and a research grant from Serono.
G. Edan has received honorariua/consulting fees from Novartis, LFB,Aventis, Serono, Bayer Schering Pharma AG; lecture grants from Biogen Idec, Serono, and grant support from Serono, Bayer Schering Pharma AG and Teva.
H.-P. Hartung has received fees for speaking at scientific symposia and honoraria for consulting ad-hoc from Bayer, Biogen Idec, Bayer Schering Pharma AG, Teva, and Serono.
D. Miller has received: honoraria/consulting fees from Biogen Idec, Wyeth, Novartis, UCB Pharma, and Bristol Myers Squibb; lecture fees from Biogen Idec and Serono and grant support from Biogen Idec, GlaxoSmithKline, and Bayer Schering Pharma AG.
X.Montalbán has received: honoraria/consulting fees, grant support and lecture fees from Biogen Idec, Wyeth, Novartis, Serono, Bayer Schering Pharma AG, Bayer Schering España SA and Teva.
F. Barkhof has served as a consultant to various pharmaceutical companies, including Aventis, Wyeth, Astra, Teva, Biogen, Bayer Schering Pharma AG, and Serono. As the director of the Image Analysis Centre, he has been remunerated for time spent conducting the blind MRI analyses.
L. Bauer, S. Dahms†, C. Pohl, and R. Sandbrink are salaried employees of Bayer Schering Pharma AG.
* Both authors contributed equally to the work.
** See the Appendix for a list of the BENEFIT Study Investigators.
Rights and permissions
About this article
Cite this article
Polman, C., Kappos, L., Freedman, M.S. et al. Subgroups of the BENEFIT study: Risk of developing MS and treatment effect of interferon beta-1b. J Neurol 255, 480–487 (2008). https://doi.org/10.1007/s00415-007-0733-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-007-0733-2