Abstract
Mitochondrial neurogastrointestinal encephalomyopathy (MNGIE) is an autosomal recessive disorder caused by mutations in the gene encoding thymidine phosphorylase (TP). Allogeneic hematopoietic stem cell transplantation (HSCT) has been proposed as a treatment for patients with MNGIE and a standardized approach to HSCT in this condition has recently been developed. We report on the transplant course, management and short-term follow-up in two MNGIE patients who underwent HSCT. The source of stem cells was bone marrow taken from an HLA 9/10 allele-matched unrelated donor in the first patient and from an HLA 10/10 allele-matched sibling donor in the second. Both patients achieved full donor chimerism, and we observed restoration of buffy coat TP activity and lowered urine nucleoside concentrations in both of them. The post-transplant clinical follow-up showed improvement in gastrointestinal dysmotility, abdominal cramps and diarrhea. Neurological assessment remained unchanged. However, the first patient died 15 months after HSCT due to gastrointestinal obstruction and shock; the second patient died 8 months after the procedure due to respiratory distress following septic shock. Although HSCT corrects biochemical abnormalities and improves gastrointestinal symptoms, the procedure can be risky in subjects already in poor medical condition as are many MNGIE patients. Since transplant-related morbidity and mortality increases with progression of the disease and number of comorbidities, MNGIE patients should be submitted to HSCT when they are still relatively healthy, in order to minimize the complications of the procedure. Anyway, there is still incomplete knowledge on the natural history of the disease in many affected patients and it is not yet clear when the best time to do a transplant is. Further clues to the therapeutic potential of HSCT could result from a prolonged observation in a greater number of non-transplanted and transplanted patients, which would allow us to answer the questions of if, how and when MNGIE patients require HSCT treatment.
Similar content being viewed by others
Introduction
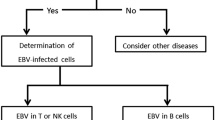
Mitochondrial neurogastrointestinal encephalomyopathy (MNGIE) is a rare autosomal recessive disorder caused by mutations of the TYMP gene encoding thymidine phosphorylase (TP), an enzyme involved in the homeostasis of the mitochondrial nucleotide pool [1]. Mutations in TYMP result in accumulation of thymidine and deoxyuridine substrates, nucleotide pool imbalance and mitochondrial DNA (mtDNA) multiple deletions, depletion and site-specific point mutations [2, 3].
Onset of symptoms occurs during the second or third decade of life and the clinical picture is characterized by external ophthalmoparesis, gastrointestinal dysmotility, cachexia, peripheral neuropathy and leukoencephalopathy [1, 2]. The relentless clinical course leads to death at a mean age of 35 years [1, 2, 4]. In recent years, treatment for MNGIE has been the object of particular attention. Replacement of TP activity by repeated platelet transfusions only produced transient and partial benefits, and administration of TP in encapsulated red cells resulted in transient reductions of plasma thymidine levels [5, 6]. Continuous ambulatory peritoneal dialysis has ameliorated vomiting and abdominal pain and permitted weight gain but symptoms presented again if dialysis was interrupted [7]. Preclinical data suggest that gene therapy is a promising therapy in MNGIE [8]. Thymidine phosphate-deficient B-lymphoblastoid cells were transduced from two MNGIE patients with lentiviral vectors, who carried a functional copy of the human TYMP DNA coding sequence. This restored TP activity in the cells, which reduced excretion of nucleoside thymidine and deoxyuridine and their concentrations when added in excess. In addition, high levels of TP activity with a concomitant reduction of nucleoside concentrations were observed in the peripheral blood of partially myeloablated double TYMP/UPP1 knockout mice treated with lentiviral-mediated hematopoietic gene therapy [8].
To date, allogeneic hematopoietic stem cell transplantation (HSCT) is the most suitable option of treatment for this otherwise intractable condition. Hematopoietic stem cell transplantation has proven to be able to restore TP activity and lower plasma nucleosides in MNGIE patients [9, 10]. A consensus conference recently proposed a common approach to HSCT in MNGIE based on standardization of the transplant protocol and the clinical and biochemical assessments that help in evaluating its safety and efficacy [10].
In this paper we report the transplant course, management and outcome of two patients with MNGIE who underwent an HSCT performed according to the consensus conference proposals, except for a few procedural changes so that it would be better tailored for the two recipients.
Case description
Patient 1
Clinical findings have already been described [11]. Briefly, the patient was a 34-year-old woman who complained of episodes of abdominal pain with alternating diarrhea and constipation over a 10-year period. At age 24, she started having a slight persistent fever, recurrent episodes of migrant arthritis, severe weight loss and episodic intestinal pseudo-obstruction often requiring parenteral nutrition. At age 31, the patient began complaining of annoying paraesthesias in her fingers and toes. A neurological examination revealed partial bilateral blepharoptosis without ophthalmoparesis, mild generalized weakness, diffuse muscle atrophy, reduced joint position and vibration sense in the lower limbs, absent ankle tendon reflexes and reduced knee jerk. An electroneurographic–electromyographic study showed a demyelinating sensory-motor polyneuropathy. Brain magnetic resonance imaging (MRI) revealed a diffuse leukoencephalopathy. Molecular analysis showed multiple mtDNA deletions and a TYMP homozygote c.1160-1G > A splice acceptor site mutation [2]. Urine thymidine and deoxyuridine assay showed abnormally elevated values and the blood TP assay was 0 nmol/mg protein/h (normal values 80–1,000).
With her informed consent, the patient underwent HSCT.
Two weeks before beginning conditioning, autologous peripheral stem cells mobilized with G-CSF alone were collected and cryopreserved as back-up. At admission, the patient’s weight was 49.5 kg (BMI 16.4) and her Karnofsky score 50. Nausea, vomiting (2–3 episodes per day), borborygmi and abdominal pain were frequent, her abdomen was sensitive to touch, diarrhea was persistent passing approximately 1,000 ml of watery stools daily.
During her hospital stay, the patient was kept in a single room with filtered air under positive pressure. Supportive therapy followed institutional protocols and included oral gut decontamination, cotrimoxazole for prophylaxis of Pneumocystis jiroveci, acyclovir for prophylaxis of herpes infections, liposomal amphotericin B for antifungal prophylaxis, and iv levetiracetam for prophylaxis of busulfan neurotoxicity. She continued total parenteral nutrition (2,000 kcal/day). The conditioning regimen was reduced in intensity, according to the international consensus conference proposals [10], and comprised iv busulfan in divided doses (0.8 mg/kg/dose, every 6 h, total dose 12.8 mg/kg) daily for 4 days (d-5 to d-2) with therapeutic drug monitoring and fludarabine 30 mg/m2 for 5 days (d-6 to d-2, total dose 150 mg/m2). Graft-versus-host disease (GvHD) prophylaxis consisted of rabbit anti-thymocyte globulins (ATG) (Genzyme), 2.5 mg/kg for 3 days (d-3 to d-1, total dose 7.5 mg/kg), cyclosporine A (CsA) with trough level monitoring and methotrexate 10 mg/m2 on days 1, 3 and 6 with leucovorin rescue.
Patient received the HSCT from an HLA 9/10 allele-matched unrelated female donor (one antigen mismatched at locus C). The stem cell source was bone marrow which was red blood cell depleted due to AB0 incompatibility. The infused product cell content was: total nucleated cells 1.97 × 108/kg, CD34+ cells 4.6 × 106/kg. The recipient was seropositive for Cytomegalovirus (CMV), whereas her donor was negative.
Engraftment was rapid with neutrophil >0.5 × 109/l by day 16 and platelets >20 × 109/l by day 17. Chimerism was assessed using semiquantitative variable nucleotide tandem repeat (VNTR) polymorphism evaluation of monocytes, and from d + 20 to the last follow-up the patient had continuously shown stable full donor chimera.
Complications observed during the early post-transplant period were fever of unknown origin (d + 7), hyperglycemia (d + 13), pancreatitis (d + 22) and CMV reactivation (d + 42 and d + 86) treated with ganciclovir. Cyclosporine A was replaced (d + 26) with mycophenolate mofetil (MMF) because of possible toxicity (headache, severe burning palmar and plantar paresthesias and lower limb pain). On d + 29 she developed an overlap GvHD syndrome with severe pancolitis requiring multiple lines of treatment over the following weeks, including iv steroids, oral budesonide, MMF, etanercept, photopheresis and mesenchymal stromal cell (MSC) infusions according to a phase I experimental protocol (Eudract 2008-007869-23). Graft-versus-host disease resolved on d + 82. On d + 93, she had a transient episode of intestinal pseudo-obstruction. The patient was discharged on d + 99 continuing treatment with steroids and photopheresis. By this time she had lost another 9 kg in weight because of gut GvHD and weighed only 40 kg (BMI 13.4). Later on, GvHD reappeared as a moderate classic chronic GvHD; [12] but after multiple lines of treatment it progressively improved and was stably mild 1 year after transplantation.
During the first year following HSCT, the patient was admitted to hospital several times to treat various complications related to immunodeficiency (hemorrhagic cystitis, pneumonia, esophagitis, stomatitis, Candida septicemia). However, 6 months after HSCT, her general conditions and gastrointestinal dysmotility had been gradually improving; nausea, vomiting, abdominal cramps and diarrhea now occurred only occasionally.
One year after HSCT, the patient still needed parenteral nutrition but she could eat small amounts of food without difficulty. No significant weight recovery was observed, in part attributable to the frequent infections and hospitalization (body weight 40 kg, BMI 13.4 kg/m2, Karnofsky score 60). She showed stable full donor chimerism and normalized lymphocyte counts: CD19+ 173/mm3 (range 100–500), CD3+ 1,420/mm3 (range 700–2,100), CD3+/CD4+ 290/mm3 (range 300–1,400), CD3+/CD8+ 1,020/mm3 (range 200–900), and CD 56+ 109/mm3 (range 90–600). Chronic GvHD was mild and she was continuing immunosuppressive treatment with only rapamycin and low-dose steroids on tapering. Neurological assessment and electroneurographic findings remained unchanged. Restored levels of TP activity were persistently observed in the patient’s peripheral blood with a concomitant striking reduction of nucleoside concentrations (Fig. 1a, b). She never had episodes of intestinal obstruction during the year following transplantation, but 15 months after the HSCT (41 kg, BMI 14.1, Karnofsky 70), she developed progressively worsening gastrointestinal symptoms (repeated vomiting and pain) and obstruction was diagnosed. She had been urgently admitted to the ICU of the hospital closest to her home, but she died after a few hours, on day +453, due to sudden shock and coma. An autopsy was not performed, but sudden shock might have been secondary to an intestinal rupture and/or an acute sepsis.
Patient 2
This patient was a 22-year-old woman who presented with recurrent abdominal pain, frequent diarrhea and vomiting, episodes of intestinal pseudo-obstruction and marked loss of weight, which she had endured since childhood. On examination, she was cachectic with a BMI of ten, had bilateral lid ptosis and ophthalmoplegia, neurosensorial deafness, diffuse muscle atrophy with severe weakness of feet dorsiflexors, reduced joint position as well as tingling in the lower limbs and absent deep tendon reflexes (Fig. 2). Electroneurography showed a severe demyelinating sensory and motor polyneuropathy and brain MRI showed a supra-tentorial leukoencephalopathy (Fig. 3a). Urine thymidine was 23.01 mmol/mol creatinine and urine deoxyuridine was 79.70 mmol/mol creatinine. No TP activity was detected in the blood. Direct sequencing of TYMP showed the homozygote c.1160-1G > A splice acceptor site mutation.
MR imaging of patient 2. a Before the transplant, notice the bilateral supra-tentorial leukoencephalopathy. b The patient goes blind. MRI shows the extent of white matter signal alterations, which now involves mostly the posterior areas and the lenticular nuclei. c The patient goes into a coma. MRI shows initial left uncal herniation
The patient received the HSCT from her brother who was HLA10/10 allele-matched, AB0 group-matched and was not a TYMP mutation carrier. She underwent HSCT following the same preparation/conditioning regimen and supportive therapy as reported above for patient one, according to the international consensus conference proposal [10]. Graft-versus-host disease prophylaxis was intensified by adding two doses of ATG (total dose 5 mg/kg) and rituximab 200 mg/m2 on d + 3, the latter also as prophylaxis against reactivating Epstein-Barr virus [13–16]. When the patient was admitted to hospital, she weighed 26 kg (BMI 12) and her Karnofsky score was 50. The infused unmanipulated marrow content was: total nucleated cells 7.4 × 108/kg, CD34+ cells 13.3 × 106/kg.
Neutrophil engraftment occurred on d + 17 and platelets on d + 14. Chimerism on d + 18 was 80 % and it was 100 % by d + 29; it did not change and was still stable at the latest follow-up.
The early post-transplant period was mostly uneventful and the patient was discharged on d + 29. During the following months she had two extremely transient episodes of mild skin and gut GvHD overlap syndrome, which were successfully treated with extracorporeal photopheresis and short-lasting low dose steroid therapy. Over the next 6 months she experienced a marked reduction of daily gastrointestinal discomfort whereas neurological assessment remained unchanged. She was readmitted to hospital only on two occasions (d + 56, d + 197) for episodes of transient intestinal pseudo-obstruction. Also in this patient, restored levels of TP activity were observed in the peripheral blood associated with a concomitant reduction of nucleoside concentrations (Fig. 1c, d). Six months after HSCT (d + 177), just as the patient was GvHD-free and continuing CsA while tapering steroids, she experienced a rapid onset of eyesight impairment characterized by blurry bilateral vision that rapidly deteriorated until she was almost blind.
Extensive tests aimed at identifying biochemical, infectious, drug or immunological disorders related to the clinical picture were negative. Optic disc swelling was not observed. Pupillary light reflexes were intact. Brain MRI showed an enlargement of the T2-weighted signal alterations that almost completely involved the supra-tentorial white matter and corpus callosum and T1- and weighted bilateral hyperintensity of the basal ganglia (Fig. 3b). No signal alterations were detected in either optic nerve.
Cyclosporine A was stopped, manganese was removed from parenteral nutrition and an empirical treatment with acyclovir (15 mg/kg every 8 h) and vitamin B1 (600 mg daily) was started without any significant improvement over the following weeks. At that time, lymphocyte subset counts had already normalized: CD19+ 411/mm3 (range 100–500), CD56+ 191/mm3 (range 90–600), CD3+/CD4+ 1,390/mm3 (range 300–1,400), CD3+/CD8+ 606/mm3 (range 200–900), and CD3+ 2,100/mm3 (range 700–2,100).
One month later (d + 205), she unexpectedly lost consciousness (Karnofsky 10, Glasgow coma scale 3). A new MRI showed hyperintense signals throughout the cerebral white matter. The posterior structures were swollen with reduced liquoral spaces and initial left uncal herniation (Fig. 3c).
We hypothesized posterior reversible encephalopathy syndrome (PRES) and treated the patient with dexamethasone. In 1 week her clinical condition had improved; the patient was awake and conscious, but blind. Two weeks later she was discharged with a slow tapering of dexamethasone. However, 8 months after HSCT (30.5 kg, BMI 14.1, Karnofsky 50), the patient was urgently readmitted to the hospital because of Clostridium difficile-related diarrhea (d + 245) followed by septic shock, preceded by an episode of transient intestinal pseudo-obstruction (d + 238) treated with antibiotics. Despite recovery of hemodynamic conditions, she died 4 days later (d + 246) due to acute respiratory distress syndrome.
Discussion
Mitochondrial neurogastrointestinal encephalomyopathy is a devastating, progressive, autosomal recessive disease caused by a defect of intergenomic signaling [1, 2]. Affected patients usually carry mutations in the TYMP gene encoding the enzyme TP and accumulate excessive amounts of thymidine and deoxyuridine in their blood [1, 2]. Gastrointestinal dysfunctions, i.e., gastrointestinal dysmotility, nausea, dysphagia, gastroesophageal reflux, postprandial emesis, abdominal pain and distention, and diarrhea are the prominent features of the disease and lead to progressive weight loss and severe cachexia [1, 2]. Patients usually die from complications of their gastrointestinal disorders and their inadequate nutritional status [1, 2, 4]. Other clinical aspects are progressive ptosis and ophthalmoparesis, demyelinating sensory-motor peripheral neuropathy and asymptomatic leukoencephalopathy as observed on brain MRI [1, 2, 11]. The diagnosis is confirmed by a family history consistent with autosomal recessive inheritance, high plasma and urine thymidine and deoxyuridine concentrations, reduced or absent TP enzyme activity in leukocytes and molecular genetic testing of TYMP [17, 18]. Recently, significant progress has been made in treating this condition and HSCT now it represents the most promising treatment option for MNGIE [10].
Hematopoietic stem cell transplantation is currently used to treat more than 50,000 people worldwide each year. Most of them have malignancies but an increasing number of patients with different inborn errors of metabolism are successfully treated by such a continuously evolving procedure [19]. In most of these diseases the rationale for use of HSCT is the repopulation of the recipient with metabolically normal donor-derived cells and the cross-correction of the defective cells by the enzyme released from the normal donor cells [20, 21].
Hematopoietic stem cell transplantation in MNGIE, by replacing the immuno-hematopoietic compartment with normal cells, is thought to correct TP deficiency thus reactivating toxic nucleoside catabolism and leading to normalization of cellular nucleotide pools [9].
The initial international experience showed that HSCT led to biochemical restoration and halted progression of the disease in surviving patients. Different conditioning regimens, GvHD prophylaxis and source of stem cells have been used [9, 22]. The main limits of the procedure appear to be frequent engraftment failure and high mortality rates (approximately 50 %) [10]. Death was mainly due to transplant-related or disease-related causes or, rather, to a combination of both [10].
An international panel of experts has proposed a common approach to HSCT in MNGIE with the aim of achieving a reliable evaluation of this therapy and promoting efficient collaborative optimization of HCST in this otherwise debilitating and fatal disease [10]. The proposed protocol tailored the best achievements in the field of transplantation to the peculiar challenges raised by this unique disorder in order to reduce the risk of transplant-related complications in patients who usually have a limited tolerance to the procedure, while maintaining adequate conditioning and immunosuppression to minimize the risk of graft rejection.
In our two patients, the transplants were carried out according to those recommendations with the exception of two issues: the selection of a 9/10 HLA-matched donor for the first patient and the administration of ATG to the second one.
The consensus suggests that, if no sibling donor can be found, an HSCT with a 10/10 allele matched unrelated donor (HLA-A, -B, -C, -DRB1 and -DQB1 phenotypically identical) is recommended. Although such careful donor selection can minimize both the risk of graft rejection and graft versus host disease, it also limits the probability of eligible patients receiving a transplant. Overall, approximately 15–30 % of patients referred for allogeneic HSCT have suitable HLA-identical sibling donors. The likelihood of identifying an HLA-matched unrelated donor varies with the patient’s specific HLA alleles and ethnicity but it might be estimated to be between 40 and 60 %. The degree of HLA mismatch could have an impact on successful engraftment rates and GvHD incidence, both of which could influence survival outcomes. A single mismatch at HLA-A, -B, -C, or -DRB1 has been associated with about a 9 % increase in mortality risk [23, 24]. Although the recommendations of the consensus proposal aim to keep the procedure as safe as possible, the difference in treatment outcomes for patients transplanted with 9/10 matched versus 10/10 matched unrelated donors remains undefined, and a 9/10 mismatched unrelated donor can be considered a viable option in selected patients affected by an otherwise fatal disorder [25, 26].
Considering the clinical history and the unrelenting fated prognosis of our first patient, we regarded as acceptable the selection of a donor mismatched at locus C, since a fully matched donor could not be found.
At the time of death, our patient had almost gotten through the critical post-transplantation period; she had stable full donor chimerism, a recovering Karnofsky, being treated only for a mild, classic chronic GvHD.
Of notice, this patient developed a GvHD involving the gut in particular. It is well known that gut damage is quite important in the pathophysiology of GvHD and leads to the activation of host antigen presenting cells and donor T cells [27]. It is likely that patients affected with MNGIE present a higher risk of developing gut GvHD because of their disease-related gut damage; therefore they require special attention for prompt and aggressive treatment of such a potentially fatal complication.
Our second patient had full donor chimera with good immuno-hematological reconstitution at time of death. Although this patient received a transplant from a matched sibling, she was in very poor medical conditions so she also received ATG in order to maximize prevention of GvHD. Many studies suggest that in cases of myeloablative donor transplants, ATG therapy can reduce the risk of GvHD without affecting negatively, and potentially improving, transplant outcomes [28, 29]. Data from the Center for International Blood and Marrow Transplant Research (CIBMTR) confirm the protective effect of ATG in regards to acute and chronic GvHD prevention also in the scenario of reduced intensity conditioning transplants while the worst outcomes reported for recipients of ATG were due to increased rates of relapse in patients with onco-hematological disorders [30]. Therefore, we felt safer adding ATG because in this cachectic patient GvHD could have been more difficult to manage and some of the drugs used in the treatment of this immune complication might not have been easily tolerated.
Following HSCT, this patient experienced only slight and transient GvHD and never developed any Epstein-Barr virus reactivation. She developed the fatal complication just as she was recovering from a severe PRES and steroids were on tapering. Posterior reversible encephalopathy syndrome is a neurological syndrome characterized by headache, seizures, visual changes, altered mental status and focal neurological signs [31]. Magnetic resonance imaging usually reveals symmetric, hyperintense lesions on T2-weighted scans, which involve the white matter in the posterior parietal, occipital, frontal and temporal lobes and in brainstem, although gray matter structures may also be affected [31]. Posterior reversible encephalopathy syndrome is usually a reversible condition observed in the setting of secondary hypertension, pre-eclampsia/eclampsia, allogeneic bone marrow transplants, organ transplants, autoimmune diseases and high dose chemotherapy and immunosuppressive drugs [31].
The blindness experienced by this patient was difficult to explain. Because several cases of CsA-associated optic neuropathy in HSCT patients have been reported so far, CsA was stopped [32]. However, the optic nerves were morphologically normal at MRI and optic disc swelling was not observed in our patient. Therefore, we believe more probable a PRES-related “cortical blindness” linked to the spreading of lesions in the occipital regions.
We speculated that the death of our second patient was expedited by multiple disease- and transplant-related events such as severe chronic cachexia, PRES-related brain involvement, immunosuppressive treatment and poor respiratory muscle function, which did not allow the patient to overcome the respiratory distress.
Although for a short-time follow-up, our findings confirmed the correction of MNGIE biochemical defects by HSCT and showed some improvement in gastrointestinal symptoms and the lack of remarkable progression in neurological impairment [33, 34].
Although both patients died following the transplant, it is difficult to determine the respective roles of the transplantation and the primary disease in causing death.
In the initial international experience with MNGIE patients, nearly 50 % of patients died after HSCT, and one to two patients out of ten required a second transplant because of primary or secondary engraftment failure [33]. In other settings, the current reported rates of transplant-related mortality (TRM) ranged from approximately 5 % in children and adolescents to 10–15 % in adults who underwent a matched, unrelated donor transplant for malignancies [29, 35].
Certainly, there are several challenges involved with the HSCT procedure, mainly the fact that our patients were already in poor medical condition with limited capacities to tolerate transplant-related complications.
According to current knowledge, since transplant-related morbidity and mortality increases with progression of the disease and number of comorbidities, transplants should be done early in the course of the disease in order to minimize the associated risks, especially the graft rejection which requires intensive immunosuppression [33].
However, presently, the rule of “early transplantation” is difficult to routinely apply in MNGIE patients. This is due to both the frequent misdiagnosis caused by the clinical heterogeneity which often delays the correct diagnosis, and the incomplete knowledge about the natural history and prognostic factors in many affected cases [11]. Mitochondrial neurogastrointestinal encephalomyopathy may present with a milder phenotype and/or a longer survival period than generally reported [11]. The course of the disease in these cases is completely unknown (progression or stability?). Further studies are necessary to clarify whether these patients should receive precocious treatment, although potentially dangerous, such as HSCT when they are still relatively healthy to minimize the side-effects of the procedure. If minimally compromised patients can be considered eligible for a standardized, reduced intensity transplant, the TRM rate could change and results significantly improve.
Finally, but not less important, we do not know what the HSCT efficacy in changing long-term clinical and neuroradiological status is. Therefore, we firmly believe that prolonged observation of the natural history of the disease in a larger number of non-transplanted and transplanted patients is mandatory. These studies could give us important clues to the therapeutic potential of HSCT in this disease and allow us to know if, how and when MNGIE patients require HSCT treatment.
References
Nishino I, Spinazzola A, Hirano M (1999) Thymidine phosphorylase gene mutations in MNGIE, a human mitochondrial disorder. Science 283:689–692
Nishino I, Spinazzola A, Papadimitriou A et al (2000) Mitochondrial neurogastrointestinal encephalomyopathy: an autosomal recessive disorder due to thymidine phosphorylase mutations. Ann Neurol 47:792–800
Nishigaki Y, Martí R, Copeland WC, Hirano M (2003) Site-specific somatic mitochondrial DNA point mutations in patients with thymidine phosphorylase deficiency. J Clin Invest 111:1913–1921
Garone C, Tadesse S, Hirano M (2011) Clinical and genetic spectrum of mitochondrial neurogastrointestinal encephalomyopathy. Brain 134:3326–3332
Lara MC, Weiss B, Illa I et al (2006) Infusion of platelets transiently reduces nucleoside overload in MNGIE. Neurology 67:1461–1463
Moran NF, Bain MD, Muquit MM, Bax BE (2008) Carrier erythrocyte entrapped thymidine phosphorylase therapy for MNGIE. Neurology 71:686–688
Yavuz H, Ozel A, Christensen M et al (2007) Treatment of mitochondrial neurogastrointestinal encephalomyopathy with dialysis. Arch Neurol 64:435–438
Torres-Torronteras J, Gómez A, Eixarch H et al (2011) Hematopoietic gene therapy restores thymidine phosphorylase activity in a cell culture and a murine model of MNGIE. Gene Ther 18:795–806
Hirano M, Martı R, Casali C et al (2006) Allogeneic stem cell transplantation corrects biochemical derangements in MNGIE. Neurology 67:1458–1460
Halter J, Schüpbach WM, Casali C et al (2011) Allogeneic hematopoietic SCT as treatment option for patients with mitochondrial neurogastrointestinal encephalomyopathy (MNGIE): a consensus conference proposal for a standardized approach. Bone Marrow Transplant 46:330–337
Filosto M, Scarpelli M, Tonin P et al (2011) Pitfalls in diagnosing mitochondrial neurogastrointestinal encephalomyopathy. J Inherit Metab Dis 34:1199–1203
Filipovich AH, Weisdorf D, Pavletic S et al (2005) National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease. I. Diagnosis and staging working group report. Biol Blood Marrow Transplant 11:945–956
Soni S, Skeens M, Gross TE et al (2009) Outcome after addition of rabbit-ATG to the standard Bu + Cy regimen for allogeneic matched sibling donor hematopoietic stem cell transplantation for hemoglobinopathies in children. Cell Ther Transplant 2:113–114
Bonifazi F, Bandini G, Colaci E et al (2009) Less extensive chronic GvHD with PBSC and ATG for sibling transplant without increase in TRM or relapse. Bone Marrow Transplant 43(Suppl 1):S10
Crocchiolo R, Castagna L, El-Cheikh J et al (2011) Prior rituximab administration is associated with reduced rate of acute GVHD after in vivo T-cell depleted transplantation in lymphoma patients. Exp Hematol 39:892–896
Dominietto A, Tedone E, Soracco M et al (2012) In vivo B-cell depletion with rituximab for alternative donor hemopoietic SCT. Bone Marrow Transplant 47:101–106
Martí R, Spinazzola A, Tadesse S, Nishino I, Nishigaki Y, Hirano M (2004) Definitive diagnosis of mitochondrial neurogastrointestinal encephalomyopathy by biochemical assays. Clin Chem 50:120–124
Shoffner JM. Mitochondrial Neurogastrointestinal Encephalopathy Disease. In: Pagon RA, Bird TC, Dolan CR, Stephens K, editors. GeneReviews (internet). University of Washington, Seattle; 1993–2005. (updated 11 May 2010)
Appelbaum FR (2007) Hematopoietic-cell transplantation at 50. N Engl J Med 357:1472–1475
Boelens JJ, Prasad VK, Tolar J, Wynn RF, Peters C (2010) Current international perspectives on hematopoietic stem cell transplantation for inherited metabolic disorders. Pediatr Clin North Am 57:123–145
Rovelli AM (2008) The controversial and changing role of hematopoietic cell transplantation for lysosomal storage disorders: an update. Bone Marrow Transplant 41:S87–S89
Scarpelli M, Cotelli MS, Mancuso M et al (2010) Current options in the treatment of mitochondrial diseases. Recent Pat CNS Drug Discov 5:203–209
Lee SJ, Klein J, Haagenson M et al (2007) High-resolution donor-recipient HLA matching contributes to the success of unrelated donor marrow transplantation. Blood 110:4576–4583
Mead AJ, Thomson KJ, Morris EC et al (2010) HLA-mismatched unrelated donors are a viable alternate graft source for allogeneic transplantation following alemtuzumab-based reduced-intensity conditioning. Blood 115:5147–5153
Kröger N, Zabelina T, Binder T et al (2009) HLA-mismatched unrelated donors as an alternative graft source for allogeneic stem cell transplantation after antithymocyte globulin-containing conditioning regimen. Biol Blood Marrow Transplant 15:454–462
Crocchiolo R, Ciceri F, Fleischhauer K et al (2009) HLA matching affects clinical outcome of adult patients undergoing haematopoietic SCT from unrelated donors: a study from the Gruppo Italiano Trapianto di Midollo Osseo and Italian Bone Marrow Donor Registry. Bone Marrow Transplant 44:571–577
Ferrara JL, Levine JE, Reddy P, Holler E (2009) Graft-versus-host disease. Lancet 373:1550–1561
Finke J, Schmoor C, Lang H et al (2003) Matched and mismatched allogeneic stem-cell transplantation from unrelated donors using combined graft-versus-host disease prophylaxis including rabbit anti-T lymphocyte globulin. J Clin Oncol 21:506–513
Finke J, Bethge WA, Schmoor C et al (2009) Standard graft-versus-host disease prophylaxis with or without anti-T-cell globulin in haematopoietic cell transplantation from matched unrelated donors: a randomised, open-label, multicentre phase 3 trial. Lancet Oncol 10:855–864
Giralt S (2011) ATG and RIC: not a good match? Blood 117:6744–6745
Bartynski WS (2008) Posterior reversible encephalopathy syndrome, part 1: fundamental imaging and clinical features. Am J Neuroradiol 29:1036–1042
Walter SH, Bertz H, Gerling J (2000) Bilateral optic neuropathy after bone marrow transplantation and cyclosporin A therapy. Graefes Arch Clin Exp Ophthalmol 238:472–476
Halter J, Schüpbach WMM, Casali C et al (2011) Allogeneic HSCT for mitochondrial neurogastrointestinal encephalomyopathy: the first promising effective treatment option in an otherwise unrelenting progressive disease? Bone Marrow Transplant 46(S1):O398 (abstract)
Sicurelli F, Carluccio MA, Toraldo F et al (2012) Clinical and biochemical improvement following HSCT in a patient with MNGIE: 1-year follow-up. J Neurol. doi:10.1007/s00415-012-6500-z
Peters C, Cornish JM, Parikh SH, Kurtzberg J (2010) Stem cell source and outcome after hematopoietic stem cell transplantation (HSCT) in children and adolescents with acute leukemia. Pediatr Clin N Am 57:27–46
Acknowledgments
All co-authors have read and agreed to the contents of this paper. We kindly thank Dr. Michio Hirano from the Department of Neurology, Columbia University Medical Center, New York, NY 10032, USA for thymidine phosphorylase biochemical assay.
Conflicts of interest
The authors declare no conflicts of interest.
Ethical standard
The study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Filosto, M., Scarpelli, M., Tonin, P. et al. Course and management of allogeneic stem cell transplantation in patients with mitochondrial neurogastrointestinal encephalomyopathy. J Neurol 259, 2699–2706 (2012). https://doi.org/10.1007/s00415-012-6572-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-012-6572-9