Abstract
Introduction
We aimed to disprove an in-hospital off-hour effect in stroke patients by adjusting for disease severity and poor prognostic findings on imaging.
Patients and methods
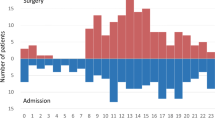
Our study included 5378 patients from a single center prospective stroke registry of a large teaching hospital in the Netherlands, admitted between January 2003 and June 2015. Patients were categorized by admission time, off-hours (OH) or working hours (WH). The in-hospital mortality, 7-day mortality, unfavorable functional outcome (modified Rankin scale > 2) and discharge to home were analyzed. Results were adjusted for age, sex, stroke severity (NIHSS score) and unfavorable findings on imaging of the brain (midline shift and dense vessel sign).
Results
Overall, 2796 patients (52%) were admitted during OH, which had a higher NIHSS score [3 (IQR 2–8) vs. 3 (IQR 2–6): p < 0.01] and had more often a dense vessel sign at admission (7.9% vs. 5.4%: p < 0.01). There was no difference in mortality between the OH-group and WH-group (6.2% vs. 6.0%; p = 0.87). The adjusted hazard ratio of in-hospital mortality during OH was 0.87 (95% CI: 0.70–1.08). Analysis of 7-day mortality showed similar results. Unadjusted, the OH-group had an unfavorable outcome [OR: 1.14 (95% CI: 1.02–1.27)] and could less frequently be discharged to home [OR: 1.16 (95% CI: 1.04–1.29)], which was no longer present after adjustment.
Discussion and conclusions
The overall outcome of stroke patients admitted to a large Dutch teaching hospital is not influenced by time of admission. When studying OH effects, adjustment for disease severity and poor prognostic findings on imaging is crucial before drawing conclusions on staffing and material.


Similar content being viewed by others
References
Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA et al (2014) Global and regional burden of stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet 383:245–254
Sorita A, Ahmed A, Starr SR, Thompson KM, Reed DA, Dabrh AM et al (2014) Off-hour presentation and outcomes in patients with acute ischemic stroke: a systematic review and meta-analysis. Eur J Intern Med 25:394–400
Saposnik G, Baibergenova A, Bayer N, Hachinski V (2007) Weekends: a dangerous time for having a stroke? Stroke 38:1211–1215
Palmer WL, Bottle A, Davie C, Vincent CA, Aylin P (2012) Dying for the weekend: a retrospective cohort study on the association between day of hospital presentation and the quality and safety of stroke care. Arch Neurol 69:1–7
Aylin P, Yunus A, Bottle A, Majeed A, Bell D (2010) Weekend mortality for emergency admissions. A large, multicentre study. Qual Saf Health Care 6:213–217
Bell CM, Redelmeier D (2001) Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med 345:663–668
Ruiz M, Bottle A, Aylin PP. The Global Comparators project: international comparison of 30-day in-hospital mortality by day of the week. BMJ Qual Saf 2015;492–504
Albright KC, Raman R, Ernstrom K, Hallevi H, Martin-Schild S, Meyer BC et al (2009) Can comprehensive stroke centers erase the “Weekend effect”? Cerebrovasc Dis 27:107–113
Albright KC, Savitz SI, Raman R, Martin-Schild S, Broderick J, Ernstrom K et al (2012) Comprehensive stroke centers and the ‘weekend effect’: the SPOTRIAS experience. Cerebrovasc Dis 34:424–429
Jauss M, Oertel W, Allendoerfer J, Misselwitz B, Hamer H (2009) Bias in request for medical care and impact on outcome during office and non-office hours in stroke patients. Eur J Neurol 10:1165–1167
Kamitani S, Nishimura K, Nakamura F, Kada A, Nakagawara J, Toyoda K et al (2014) Consciousness level and off-hour admission affect discharge outcome of acute stroke patients: a J-ASPECT study. J Am Heart Assoc 3:e001059
Kim SC, Hong KS, Hwang SI, Kim JE, Kim AR, Cho JY et al (2012) Weekend admission in patients with acute ischemic stroke is not associated with poor functional outcome than weekday admission. J Clin Neurol 8:265–270
Kim C, Jang MU, Oh MS, Park JH, Jung S, Lee JH et al (2014) Off-hour effect on 3-month functional outcome after acute ischemic stroke: a prospective multicenter registry. PLoS One 9:e105799
Kristiansen NS, Mainz J, Norgard BM, Bartels PD, Andersen G, Johnsen SP (2014) Off-hours admission and acute stroke care quality: a nationwide study of performance measures and case-fatality. Stroke 45:3663–3669
Martínez-Martínez MM, Fernández-Travieso J, Fuentes B, Ruiz-Ares G, Martínez-Sánchez P, García RC et al (2012) Off-hour effects on stroke care and outcome in stroke centres. Eur J Neurol 08:1140–1145
Streifler JY, Benderly M, Molshatzki N, Bornstein N, Tanne D (2012) Off-hours admission for acute stroke is not associated with worse outcome—a nationwide Israeli stroke project. Eur J Neurol 04:643–647
Fang JS, Saposnik G, Silver FL, Kapral MK (2010) Investigators of the Registry of the Canadian Stroke Network. Association between weekend hospital presentation and stroke fatality. Neurology 75:1589–1596
Hasegawa Y, Yoneda Y, Okuda S, Hamada R, Toyota A, Gotoh G et al (2005) The effect of weekends and holidays on stroke outcome in acute stroke units. Cerebrovasc Dis 20:325–331
Lee J, Morishima T, Kunisawa S, Sasaki N, Otsubo T, Ikai H et al (2013) Derivation and validation of in-hospital mortality prediction models in ischaemic stroke patients using administrative data. Cerebrovasc Dis 35:73–80
Niewada M, Jezierska-Ostapczuk A, Skowronska M, Sarzynska-Dlugosz I, Czlonkowska A (2012) Weekend versus weekday admissions in polish stroke centres—could admission day affect prognosis in polish ischaemic stroke patients? Neurol Neurochir Pol 46:15–21
Bray BD, Cloud GC, James MA, Hemingway H, Paley L, Stewart K et al (2016) Weekly variation in health-care quality by day and time of admission: a nationwide, registry-based, prospective cohort study of acute stroke care. Lancet 388(10040):170–177
Cho KH, Park EC, Nam CM, Choi Y, Shin J, Lee SG (2016) Effect of weekend admission on in-hospital mortality in patients with ischemic stroke: an analysis of Korean nationwide claims data from 2002 to 2013. J Stroke Cerebrovasc Dis 25(2):419–427
Turner M, Barber M, Dodds H, Dennis M, Langhorne P, Macleod MJ (2016) Stroke patients admitted within normal working hours are more likely to achieve process standards and to have better outcomes. J Neurol Neurosurg Psychiatry 87(2):138–143
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19:604–607
Adams HP Jr, Davis PH, Leira EC, Chang KC, Bendixen BH, Clarke WR et al (1999) Baseline NIH stroke scale score strongly predicts outcome after stroke: a report of the Trial of Org 10172 in acute stroke treatment (TOAST). Neurology 53:126–131
Nedeltchev K, Renz N, Karameshev A, Haefeli T, Brekenfeld C, Meier N et al (2010) Predictors of early mortality after acute ischaemic stroke. Swiss Med Wkly 140:254–259
Braga P, Ibarra A, Rega I, Ketzoian C, Pebet M, Servente L et al (2002) Prediction of early mortality after acute stroke. J Stroke Cerebrovasc Dis 11:15–22
Bakshi R, Mazziotta JC (1998) Acute middle cerebral artery thrombosis demonstrated by cranial computed tomography: the “dense MCA” sign. Arch Neurol 55:1577
Curtze S, Meretoja A, Mustanoja S, Putaala J, Lindberg T, Leppä M et al (2012) Does time of day or physician experience affect outcome of acute ischemic stroke patients treated with thrombolysis? A study from Finland. Int J Stroke 7:511–516
Cram P, Hillis SL, Barnett M, Rosentahal GE (2004) Effects of weekend admission and hospital teaching status on in-hospital mortality. Am J Med 117:151–157
McKinney JS, Deng Y, Kasner SE, Kostis JB (2011) Comprehensive stroke centers overcome the weekend versus weekday gap in stroke treatment and mortality. Stroke 9:2403–2409
Reeves MJ, Smith E, Fonarow G, Hernandez A, Pan W, Schwamm LH (2009) Off-hour admission and in-hospital stroke case fatality in the get with the guidelines—stroke program. Stroke 40:569–576
Tung YC, Chang GM, Chen YH (2009) Associations of physician volume and weekend admissions with ischemic stroke outcome in Taiwan: a nationwide population-based study. Med Care 09:1018–1025
Ogbu UC, Westert GP, Slobbe LCJ, Stronks K, Arah OA (2011) A multifaceted look at time of admission and its impact on case-fatality among a cohort of ischaemic stroke patients. J Neurol Neurosurg Psychiatry 1:8–13
Fang K, Churilov L, Weir L, Dong Q, Davis S, Yan B (2014) Thrombolysis for acute ischemic stroke: do patients treated out of hours have a worse outcome? J Stroke Cerebrovasc Dis 23(3):427–432
Nakajima M, Inatomi Y, Yonehara T, Watanabe M, Ando Y (2015) Outcome in patients admitted outside regular hospital working hours: does time until regular working hours matter? Int J Stroke 10:79–84
Hoh BL, Chi YY, Waters MF, Mocco J, Barker FG (2010) Effect of weekend compared with weekday stroke admission on thrombolytic use, in-hospital mortality, discharge disposition, hospital charges, and length of stay in the nationwide inpatient sample database, 2002–2007. Stroke 41:2323–2328
Turin TC, Kita Y, Rumana N, Ichikawa M, Sugihara H, Morita Y et al (2008) Case fatality of stroke and day of the week: is the weekend effect an artifact? Takashima stroke registry, Japan (1988–2003). Cerebrovasc Dis 26:606–611
Ayanian JZ, Weissman JS (2002) Teaching hospitals and quality of care: a review of the literature. Milbank Q 80:569–593
Saad A, Adil MM, Patel V, Owada K, Winningham MJ, Nahab F (2014) Clinical outcomes after thrombectomy for acute ischemic stroke on weekends versus weekdays. J Stroke Cerebrovasc Dis 23:2708–2713
Scholte op Reimer WJ, Dippel DW, Franke CL, van Oostenbrugge RJ, de Jong G, Hoeks S et al (2006) Quality of hospital and outpatient care after stroke or transient ischemic attack: insights from a stroke survey in the Netherlands. Stroke 37:1844–1849
Jungehulsing GJ, Rossnagel K, Nolte CH, Muller-Nordhorn J, Roll S, Klein M et al (2006) Emergency department delays in acute stroke—analysis of time between ED arrival and imaging. Eur J Neurol 13:225–232
Rose KM, Rosamond WD, Huston SL, Murphy CV, Tegeler CH (2008) Predictors of time from hospital arrival to initial brain-imaging among suspected stroke patients: the North Carolina Collaborative Stroke Registry. Stroke 12:39:3262–3267
Madej-Fermo OP, Staff I, Fortunato G, Abbott L, McCullough LD (2012) Impact of emergency department transitions of care on thrombolytic use in acute ischemic stroke. Stroke 43:1067–1074
Bodenant M, Leys D, Debette S, Cordonnier C, Dumont F, Henon H et al (2010) Intravenous thrombolysis for acute cerebral ischaemia: comparison of outcomes between patients treated at working versus nonworking hours. Cerebrovasc Dis 30:148–156
Crowley RW, Yeoh HK, Stukenborg GJ, Medel R, Kassell NF, Dumont AS (2009) Influence of weekend hospital admission on short-term mortality after intracerebral hemorrhage. Stroke 40:2387–2392
Kazley AS, Hillman DG, Johnston KC, Simpson KN (2010) Hospital care for patients experiencing weekend vs weekday stroke: a comparison of quality and aggressiveness of care. Arch Neurol 67:39–44
De Bruin A, De Bruin EL, Gast A, Kardaun JWPF, Sijl M, Verweij GCG (2003) Koppeling van LMR-en GBA gegevens: methode, resultanten en kwaliteitsonderzoek. CBS, Heerlen, The Netherlands
McCormick N, Bhole V, Lacaille D, Avina-Zubieta JA (2015) Validity of diagnostic codes for acute stroke in administrative databases: a systematic review. PLoS One 10:e0135834
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that there is no conflict of interest. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethical standard
Neither an ethical approval nor an informed consent was sought for this article because this study is a retrospective cohort study of anonymously collected data. This study was completed in accordance with the Helsinki Declaration as revised in 2013.
Rights and permissions
About this article
Cite this article
Tuinman, M.P., van Golde, E.G.A., Portier, R.P. et al. Comparison of outcome in stroke patients admitted during working hours vs. off-hours; a single-center cohort study. J Neurol 266, 782–789 (2019). https://doi.org/10.1007/s00415-018-9079-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-018-9079-1