Abstract
Purpose
This study describes a standardized screening protocol for diagnosis of invasive mold infections in pediatric oncology patients with neutropenia and prolonged or recurrent fever.
Methods
A retrospective chart review was performed of children receiving intensive chemotherapy for hematologic malignancies who developed invasive mold infections from 2004 to 2011. Characteristics and outcomes were compared before and after implementation of the screening protocol in November 2006. The screen includes direct nasal endoscopy performed at the bedside by an otorhinolaryngologist, noncontrast computed tomography (CT) of the chest, and abdominal ultrasound in patients with neutropenia and prolonged or recurrent fever.
Results
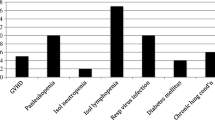
Fifty patients had proven, probable, or possible invasive mold infections. Before routine use of direct nasal endoscopy, invasive nasosinal disease was detected in 5 of 19 patients (26 %) and all had a compatible clinical presentation. Thirteen of 31 patients (42 %) in the post-screen group had nasosinal disease, and fever was the only sign for 8 patients (62 %). Twenty-four patients with nasosinal disease had a sinus CT, and radiologic findings of bony erosion or peri-sinus invasion were never detected. Eight of 19 patients in the pre-screen group died from mold infection (42.1 %) versus 4 of 31 (12.9 %) in the post-screen group (p = 0.04).
Conclusions
A screening protocol including direct nasal endoscopy, noncontrast chest CT, and abdominal ultrasound was effective in detecting invasive mold infections in at-risk patients. Nasosinal involvement often occurs before specific symptoms develop, and sinus CTs are insensitive and nonspecific. Bedside nasal endoscopy precludes radiation exposure associated with sinus CT and was associated with decrease in mold-related mortality, likely due to earlier diagnosis and initiation of appropriate antifungal therapy.
Similar content being viewed by others
References
Rosen GP et al. (2005) Invasive fungal infections in pediatric oncology patients: 11 year experience at a single institution. J Pediatr Hematol Oncol 27(3):135–140
Mor M, Gilad G, Kornreich L, Fisher S, Yaniv I, Levy I (2011) Invasive fungal infections in pediatric oncology. Pediatr Blood Cancer 56:1092–1097
Castagnola et al. Fungal infections in children with cancer. A prospective, multicenter surveillance study. 2006: 25(7):634–39
Kobayashi R, Kaneda M, Sato T, et al. (2008) The clinical feature of invasive fungal infection in pediatric patients with hematologic and malignant diseases. A 10-year analysis at a single institution at Japan. J Pediatr Hematol Oncol 30:886–890
Grigull L et al. (2003) Invasive fungal infections are responsible for one-fifth of the infectious deaths in children with ALL. Mycoses 46:441–446
Groppo E, El-Sayed I, Aiken A, Glastonbury C (2011) Magnetic resonance imaging characteristics of acute invasive fungal sinusitis. Arch Otolaryngol Head Neck Surg. 137(10):1005–1010
DelGaudio JM, Clemson LA (2009) An early detection protocol for invasive fungal sinusitis in neutropenic patients successfully reduces extent of disease at presentation and long term morbidity. Laryngoscope 119:180–183
DelGaudio JM, Swain RE, Kingdom TT, Muller S, Hudgins PA (2003) Computed tomographic findings in patients with invasive fungal sinusitis. Arch Otolaryngol Head Neck Surg 129:236–240
De Pauw B et al. (2008) Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis 46(12):1813–1821
Park AH, Muntz HR, Smith ME, Afify Z, Pysher T, Pavia A (2005) Pediatric invasive fungal rhinosinusitis in immunocompromised children with cancer. Otolaryngol Head Neck Surg 133:411–416
Lehrnbecher T, Phillips R, Alexander S, Alvaro F, Carlesse F, Fisher B, Hakim H, Sanolaya M, Castagnola E, Davis B, Dupuis L, Gibson F, Groll A, Gaur A, Gupta A, Kebudi R, Petrilli S, Steinbach W, Villarroel M, Zaoutis T, Sung L (2012) Guideline for the management of fever and neutropenia in children with cancer and/or undergoing hematopoietic stem-cell transplantation. J Clin Oncol 30:4427–4438
Rassi SJ, Melkane AE, Rizk HG, Dahoui HA (2009) Sinonasal mucormycosis in immunocompromised pediatric patients. J Pediatr Hematol Oncol 31(12):907–910
Ardeshirpour F et al. (2014) Surgery for pediatric invasive fungal Sinonasal disease. Laryngoscope 124:1008–1012
Milito MA, Kontoyiannis DP, Lewis RE, Liu P, Mawlawi OR, Truong MT, Marom EM (2010) Influence of host immunosuppression on CT findings in invasive pulmonary aspergillosis. Med Mycol 48(6):817–823
Burgos A, Zaoutis TE, Dvorak CC, Hoffman JA, Knapp KM, Nania JJ, Prasad P, Steinbach WJ (2008) Pediatric invasive aspergillosis: a multicenter retrospective analysis of 139 contemporary cases. Pediatrics 121(5):e1286–e1294
Agrawal AK, Saini N, Gildengorin G, Feusner JH (2001) Is routine computed tomography scanning justified in the first week of persistent febrile neutropenia in children with malignancies? Pediatr Blood Cancer 57:620–624
Lambert J, MacKenzie JD, Cody D, Gould R (2014) Techniques and tactics for optimizing CT dose in adults and children: state of the art and future advances. J Am Coll Radiol 11:262–266
Raman SP, Johnson PT, Deshmukh S, Mahesh M, Grant KL, Fishman EK (2013) CT dose reduction applications: available tools on the latest generation of CT scanners. J Am Coll Radiol 10:37–41
Nelson TR (2014) Practical strategies to reduce pediatric CT radiation dose. J Am Coll Radiol 11:292–299
Castagnola E, Bagnasco F, Amoroso L, Caviglia I, Caruso S, Faraci M, Cavillo M, Moroni C, Bandettini R, Cangegmi G, Magnano GM, Buffa P, Moscatelli A, Haupt R (2014) Role of management strategies in reducing mortality from invasive fungal disease in children with cancer or receiving hematopoietic stem cell transplant. Pediatr Infect Dis J 33(3):233–237
Wingard JR, Hiemenz JW, Jantz MA (2012) How I manage pulmonary nodular lesions and nodular infiltrates in patients with hematologic malignancies or undergoing hematopoietic stem cell transplantation. Blood 120(9):1791–1800
Franquet T, Rodriguez S, Martino R, Salinas T, Giménez A, Hidalgo A (2005) Human metapneumovirus infection in hematopoietic stem cell transplant recipients: high-resolution computed tomography findings. J Comput Assist Tomogr 29(2):223–227
Franquet T, Müller NL, Giménez A, Martínez S, Madrid M, Domingo P. Infectious pulmonary nodules in immunocompromised patients: usefulness of computed tomography in predicting their etiology. J Comput Assist Tomogr 2003: 27(4): 461–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Cohn, S.M., Pokala, H.R., Siegel, J.D. et al. Application of a standardized screening protocol for diagnosis of invasive mold infections in children with hematologic malignancies. Support Care Cancer 24, 5025–5033 (2016). https://doi.org/10.1007/s00520-016-3367-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3367-z