Abstract
Background
Deep brain stimulation (DBS) of the sub-thalamic nucleus (STN) is a recognised treatment for advanced Parkinson’s disease (PD). We present our results of 10 consecutive patients implanted under general anaesthesia (GA) using intraoperative robotic three-dimensional (3D) fluoroscopy (Artis Zeego; Siemens, Erlangen, Germany).
Method
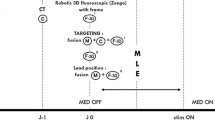
Ten patients (nine men, one woman) with a mean age of 57.6 (range, 41–67) years underwent surgery between October 2013 and January 2015. The mean duration of PD was 9.2 [1–10] year. The procedure was performed under GA: placement of the stereotactic frame, implantation of the electrodes (Lead 3389; Medtronic, Minnesota, MN, USA) and 3D intraoperative fluoroscopic control (Artis Zeego) with image fusion with the preoperative MRI scans. All patients were evaluated preoperatively and 6 months postoperatively.
Results
The mean operative time was 240.1 (185–325) min. The mean Unified Parkinson’s Disease Rating Scale (UPDRS) II OFF medication decreased from 23.9 preoperatively to 15.7 postoperatively. The mean OFF medication UPDRS III decreased from 41 to 11.6 and the UPDRS IV decreased from 10.6 to 7. The mean preoperative and postoperative L-Dopa doses were 1,178.5 and 696.5 mg, respectively. Two complications were recorded: one episode of transient confusion (24 h) and one internal pulse generator (IPG) infection.
Conclusions
With improvement in preoperative magnetic resonance imaging (MRI) and the ability to control the position of the leads intraoperatively using Artis Zeego, we now perform this procedure under GA. Our results are comparable to others reported. The significant decrease in the duration of surgery could be associated with a reduced rate of complications (infection, loss of patient collaboration). However, this observation needs to be confirmed.



Similar content being viewed by others
References
Fiegele T, Feuchtner G, Sohm F, Bauer R, Anton JVF, Gotwald T, Twerdy K, Eisner W (2008) Accuracy of stereotactic electrode placement in deep brain stimulation by intraoperative computed tomography. Parkinsonism Relat Disord 14:595–599
Foltynie T, Zrinzo L, Martines-Torres I, Tripoliti E, Petersen I, Holl E, Aviles-Olmos I, Jahanshahi M, Hariz M, Limousin P (2011) MRI-guided STN DBS in Parkinson’s disease without microelectrode recording: efficacy and safety. J Neurol Neurosurg Psychiatry 82:358–363
Hamid NA, Mitchell RD, Mocroft P, Westby GW, Milner J, Pall H (2005) Targeting the subthalamic nucleus for deep brain stimulation: technical approach and fusion of pre- and postoperative MR images to define accuracy of lead placement. J Neurol Neurosurg Psychiatry 76(3):409–14
Holl E, Petersen E, Foltynie T, Martinez-Torres I, Limousin P, Hariz M, Zrinzo L (2010) Improving targeting in image-guided frame-based deep brain stimulation. Neurosurgery 67(2 Suppl Operative):437–447
Holloway K, Docef A (2013) A quantitative assessment of the accuracy and reliability of O-arm images for deep brain stimulation surgery. Neurosurgery 72(1 Suppl Operative):47–57
Lee DJ, Zwienenberg-Lee M, Seyal M, Shahlaie K (2015) Intraoperative computed tomography for intracranial electrode implantation surgery in medically refractory epilepsy. J Neurosurg 122(3):526–531
Maldonado IL, Roujeau T, Cif L, Gonzalez V, El-Fertit H, Vasques X, Bonafe A, Coubes P (2009) Magnetic resonance-based deep brain stimulation technique: a series of 478 Consecutive implanted electrodes with no perioperative intracerebral hemorrhage. Neurosurgery 65(1 Suppl Operative):196–202
Maltête D, Navarro S, Welter ML, Roche S, Bonnet AM, Houeto JL, Mesnage V, Pidoux B, Dormont D, Cornu P, Agid Y (2004) Subthalamic stimulation in parkinson disease: with or without anesthesia? Arch Neurol 691(3):390–392
Mirzadeh Z, Chapple K, Lambert M, Dhall R, Ponce F (2014) Validation of Ct-MRI fusion for intraoperative assessment of stereotactic accuracy in DBS surgery. Mov Disord 29(14):1788–1794
Moll CK, Payer S, Gulberti A, Sharrott A, Zittel S, Boelmans K, Köppen J, Gerloff C, Westphal M, Engel AK, Oehlwein C, Buhmann C, Hamel W (2013) STN stimulation in general anaesthesia: evidence beyond ‘evidence-based medicine’. Acta Neurochir Suppl 117:19–25
Alterman RL, Weisz D (2012) Microelectrode recording during deep brain stimulation and ablative procedures. Mov Disord 287:1347–1391
Shahlaie K, Larson PS, Starr PA (2011) Intraoperative computed tomography for deep brain stimulation surgery: technique and accuracy assessment. Neurosurgery 68(1 Suppl Operative):114–124
Weaver FM, Follett K, Stern M, Hur K, Harris C, Marks WJ Jr, Rothlind J, Sagher O, Reda D, Moy CS, Pahwa R, Burchiel K, Hogarth P, Lai EC, Duda JE, Holloway K, Samii A, Horn S, Bronstein J, Stoner G, Heemskerk J, Huang GD, CSP 468 Study Group (2009) Bilateral deep brain stimulation vs best medical therapy for patients with advanced Parkinson disease: a randomized controlled trial. JAMA 3001:63–73
Burchiel KJ, McCartney S, Lee A, Raslan AM (2013) Accuracy of deep brain stimulation electrode placement using intraoperative computed tomography without microelectrode recording. J Neurosurg 119(2):301–6
Burchiel KJ, Anderson VC, Favre J, Hammerstad JP (1999) Comparison of pallidal and subthalamic nucleus deep brain stimulation for advanced Parkinson’s disease: results of a randomized, blinded pilot study. Neurosurgery 45:1375–1382
Deuschl G, Schade-Brittinger C, Krack P, Volkmann J, Schäfer H, Bötzel K, Daniels C, Deutschländer A, Dillmann U, Eisner W, Gruber D, Hamel W, Herzog J, Hilker R, Klebe S, Kloss M, Koy J, Krause M, Kupsch A, Lorenz D, Lorenzl S, Mehdorn HM, Moringlane JR, Oertel W, Pinsker MO, Reichmann H, Reuss A, Schneider GH, Schnitzler A, Steude U, Sturm V, Timmermann L, Tronnier V, Trottenberg T, Wojtecki L, Wolf E, Poewe W, Voges J, German Parkinson Study Group, Neurostimulation Section (2006) A randomized trial of deep brain stimulation for Parkinson’s disease. N Engl J Med 355:896–908
Patel NK, Plaha P, O’Sullivan K, McCartner R, Heywood P, Gill SS (2003) MRI directed bilateral stimulation of the subthalamic nucleus in patients with Parkinson’s disease. J Neurol Neurosurg Psychiatry 74:1631–1637
Patel NK, Plaha P, Gill SS (2007) Magnetic resonance imaging-directed method for functional neurosurgery using implantable guide tubes. Neurosurgery 61(2 Suppl Operative):358–366
Sutcliffe AJ, Gan YC, Mitchell RD, Mocroft AP, Nightingale P (2011) General anaesthesia for deep brain stimulator electrode insertion in Parkinson’s disease. Acta Neurochir 153:621–627
Montgomery EB Jr (2012) Microelectrode targeting of the subthalamic nucleus for deep brain stimulation surgery. Mov Disord 27:1387–1391
Sillay KA, Rusy D, Buyan-Dent L, Ninman NL, Vigen KK (2014) Wide-bore 1.5T MRI-guided deep brain stimulation surgery: initial experience and technique comparison. Clin Neurol Neurosurg 127:79–85
Binder DK, Rau GM, Starr PA (2005) Risk factor for hemorrhage during microelectrode-guided deep brain stimumlator implantation for movement disorders. Neurosurgery 56(4):722–732
Pahwa R, Lyons KE (2013) Handbook of Parkinson’s disease, 5th edn. CRC Press, Boca Raton
Schuepbach WM, Rau J, Knudsen K, Volkmann J, Krack P, Timmermann L, Hälbig TD, Hesekamp H, Navarro SM, Meier N, Falk D, Mehdorn M, Paschen S, Maarouf M, Barbe MT, Fink GR, Kupsch A, Gruber D, Schneider GH, Seigneuret E, Kistner A, Chaynes P, Ory-Magne F, Brefel Courbon C, Vesper J, Schnitzler A, Wojtecki L, Houeto JL, Bataille B, Maltête D, Damier P, Raoul S, Sixel-Doering F, Hellwig D, Gharabaghi A, Krüger R, Pinsker MO, Amtage F, Régis JM, Witjas T, Thobois S, Mertens P, Kloss M, Hartmann A, Oertel WH, Post B, Speelman H, Agid Y, Schade-Brittinger C, Deuschl G, EARLYSTIM Study Group (2013) Neurostimulation for Parkinson’s disease with early motor complications. N Engl J Med 368:610–622
Zhang J, Weir V, Fajardo L, Lin J, Hsiung H, Ritenour ER (2009) Dosimetric characterization of a cone-beam O-arm imaging system. J Xray Sci Technol 17(4):305–317
Zrinzo L, Foltynie T, Limousin P, Hariz M (2012) Image-verified deep brain stimulation reduces risk and cost with no apparent impact on efficacy. Mov Disord 27(12):1585–1586
Zrinzo L, Foltynie T, Limousin P, Hariz M (2012) Reducing hemorrhagic complications in functional neurosurgery: a large case series and systematic literature review. J Neurosurg 116:84–94
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organisation or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
For this type of study formal consent is not required.
Informed consent
Informed consent was obtained from all individual participant
Rights and permissions
About this article
Cite this article
Delavallée, M., Delaunois, J., Ruwet, J. et al. STN DBS for Parkinson’s disease: results from a series of ten consecutive patients implanted under general anaesthesia with intraoperative use of 3D fluoroscopy to control lead placement. Acta Neurochir 158, 1783–1788 (2016). https://doi.org/10.1007/s00701-016-2889-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-016-2889-y