Abstract
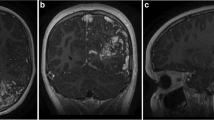
A subgroup of patients initially treated by radiosurgery underwent surgical resection because of recurrent hemorrhage or neurological deterioration. In a retrospective study, we want to analyze the clinical features of these patients and evaluate the effect of microneurosurgery in such rare constellations. Moreover, we hope to find answers about failure of radiation therapy in these cases by correlation of radiobiological and histopathological data. Over a 16-year-period, eight patients with cerebral arteriovenous malformation (AVM) underwent surgical resection, who previously were treated by radiosurgery. The mean duration between radiation therapy and final resection was 7 years. Preoperative evaluation revealed Spetzler–Martin grade III (n = 5) and IV (n = 3) AVMs. Histological examination was achieved in all resected lesions. Mean neurological follow-up was 14 months. Indications for surgical resection were intracerebral hematoma, progressive neurological deficit, and epilepsy. In comparison to the initial angiographic study before radiation therapy, preoperative angiography revealed newly developed “en passant” feeding vessels and stenosis of the main venous drainage in some patients. The mean Rankin score for all patients was 2.75 before and 3.25 after surgical resection. Postoperatively, three patients (38%) developed neurological deterioration. Histological examination of the resected tissue revealed significant radiation-induced pathology in six patients. We did not see correlation between radiation doses and severity of histolopathological radiation-induced changes. Postoperative angiography confirmed total AVM resection in all patients. AVMs insufficiently treated by radiation bear an increased surgical risk. Often, angiographic studies revealed a more complicated morphology. Microsurgical resection was extremely challenging and led to unfavorable outcomes in many of the patients.



Similar content being viewed by others
References
Asgari S, Rohrborn HJ, Engelhorn T, Fauser B, Stolke D (2003) Intraoperative measurement of cortical oxygen saturation and blood volume adjacent to cerebral arteriovenous malformations using near-infrared spectroscopy. Neurosurgery 52:1298–1304 discussion 1304-1296
Barker FG 2nd, Butler WE, Lyons S, Cascio E, Ogilvy CS, Loeffler JS, Chapman PH (2003) Dose-volume prediction of radiation-related complications after proton beam radiosurgery for cerebral arteriovenous malformations. J Neurosurg 99:254–263
Bonita R, Beaglehole R (1988) Recovery of motor function after stroke. Stroke 19:1497–1500
Flickinger JC, Lundsford LD, Kondziolka D (1991) Dose prescription and dose-volume effects in radiosurgery. Neurosurg Clin North Am 3:51–59
Foote KD, Friedman WA, Ellis TL, Bova FJ, Buatti JM, Meeks SL (2003) Salvage retreatment after failure of radiosurgery in patients with arteriovenous malformations. J Neurosurg 98:337–341
Friedman WA, Bova FJ (1992) Linear accelerator radiosurgery for arteriovenous malformations. J Neurosurg 77:832–841
Kaufman M, Swartz BE, Mandelkern M, Ropchan J, Gee M, Blahd WH (1990) Diagnosis of delayed cerebral radiation necrosis following proton beam therapy. Arch Neurol 47:474–476
Kjellberg RN, Davis KR, Lyons S, Butler W, Adams RD (1984) Bragg peak proton beam therapy for arteriovenous malformation of the brain. Clin Neurosurg 31:248–290
Laing RW, Childs J, Brada M (1992) Failure of conventionally fractionated radiotherapy to decrease the risk of hemorrhage in inoperable arteriovenous malformations. Neurosurgery 30:872–875 discussion 875-876
Lunsford LD (2003) Proton beam for arteriovenous malformations.[comment]. J Neurosurg 99:222–223 discussion 223-224
Lunsford LD, Kondziolka D, Flickinger JC, Bissonette DJ, Jungreis CA, Maitz AH, Horton JA, Coffey RJ (1991) Stereotactic radiosurgery for arteriovenous malformations of the brain. J Neurosurg 75:512–524
Maesawa S, Flickinger JC, Kondziolka D, Lunsford LD (2000) Repeated radiosurgery for incompletely obliterated arteriovenous malformations. J Neurosurg 92:961–970
Massengale JL, Levy RP, Marcellus M, Moes G, Marks MP, Steinberg GK (2006) Outcomes of surgery for resection of regions of symptomatic radiation injury after stereotactic radiosurgery for arteriovenous malformations. Neurosurgery 59:553–560 discussion 553-560
Pollock BE, Flickinger JC, Lunsford LD, Maitz A, Kondziolka D (1998) Factors associated with successful arteriovenous malformation radiosurgery. Neurosurgery 42:1239–1244 discussion 1244-1237
Pollock BE, Gorman DA, Coffey RJ (2003) Patient outcomes after arteriovenous malformation radiosurgical management: results based on a 5- to 14-year follow-up study. Neurosurgery 52:1291–1296 discussion 1296-1297
Pollock BE, Lunsford LD, Kondziolka D, Maitz A, Flickinger JC (1994) Patient outcomes after stereotactic radiosurgery for “operable” arteriovenous malformations. Neurosurgery 35:1–7 discussion 7-8
Redekop GJ, Elisevich KV, Gaspar LE, Wiese KP, Drake CG (1993) Conventional radiation therapy of intracranial arteriovenous malformations: long-term results. J Neurosurg 78:413–422
Schneider BF, Eberhard DA, Steiner LE (1997) Histopathology of arteriovenous malformations after gamma knife radiosurgery. J Neurosurg 87:352–357
Seifert V, Stolke D, Mehdorn HM, Hoffmann B (1994) Clinical and radiological evaluation of long-term results of stereotactic proton beam radiosurgery in patients with cerebral arteriovenous malformations. J Neurosurg 81:683–689
Statham P, Macpherson P, Johnston R, Forster DM, Adams JH, Todd NV (1990) Cerebral radiation necrosis complicating stereotactic radiosurgery for arteriovenous malformation. J Neurol Neurosurg Psychiatry 53:476–479
Steinberg GK, Chang SD, Levy RP, Marks MP, Frankel K, Marcellus M (1996) Surgical resection of large incompletely treated intracranial arteriovenous malformations following stereotactic radiosurgery. J Neurosurg 84:920–928
Sure U, Battenberg E, Dempfle A, Tirakotai W, Bien S, Bertalanffy H (2004) Hypoxia-inducible factor and vascular endothelial growth factor are expressed more frequently in embolized than in nonembolized cerebral arteriovenous malformations. Neurosurgery 55:663–669 discussion 669-670
Yamamoto M, Jimbo M, Hara M, Saito I, Mori K (1996) Gamma knife radiosurgery for arteriovenous malformations: long-term follow-up results focusing on complications occurring more than 5 years after irradiation. Neurosurgery 38:906–914
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Ludwig Benes, Marburg, Germany
In this retrospective study, Asgari and coworkers comment on a subset of eight AVM patients, out of a group of 440 individuals, who underwent AVM resection in one department, experiencing recurrent hemorrhage or neurological deterioration after initial radiation therapy.
During the last years, not much is written upon this challenging topic, and there are only few substantial management recommendations published in the pertinent literature.
The implication of this study is that AVMs insufficiently treated by radiation therapy hold an increased risk for additional morbidity and mortality not referred to in the Spetzler and Martin grading system. This paper reminds us that hemorrhage during radiation therapy is still a controversy in terms of using repetitive radiation or surgical therapy. Personally, I have good experiences in some individuals suffering from large AVMs with a deeply located part close to the ventricles, when radiation therapy starts with the “ventricular cone” followed by subsequent surgical resection of the superficially located rest of the AVM nidus several months later. In selected patients, this strategy was beneficial in reducing bleeding complications from these AVMs.
This well-written article is an additional and valuable contribution to the controversy of AVM resection after previously performed radiation therapy.
Tatsuki Oyoshi, Zurich, Switzerland
The authors reported eight AVM patients, who underwent AVM resection in their department presenting neurological deterioration or recurrent hemorrhage after initial radiation therapy.
They indicated that microneurosurgical resection for the patient with incompletely treated AVM after initial radiosurgery is very challenging and led to unfavorable outcomes in most cases. Recently, radiotherapy has been advocated in high-risk AVM, such as located in eloquent area, deep seated area, or large size. However, the long-term complications of radiation therapy, including radiation necrosis, cyst formation, hemorrhage, recanalization, increased seizure frequency, and arterial stenosis, occur in some patients who undergo radiation therapy for AVM. This paper would suggest the importance of a selection of treatment modality in high-risk AVM. Of course, follow-up angiography is mandatory for the patients with incompletely treated AVM after radiotherapy.
Rights and permissions
About this article
Cite this article
Asgari, S., Bassiouni, H., Gizewski, E. et al. AVM resection after radiation therapy—clinico-morphological features and microsurgical results. Neurosurg Rev 33, 53–61 (2010). https://doi.org/10.1007/s10143-009-0216-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-009-0216-2