Abstract
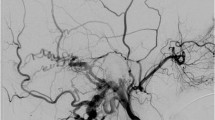
We reviewed the anatomy and embryology of the bridging and emissary veins aiming to elucidate aspects related to the cranial dural arteriovenous fistulae. Data from relevant articles on the anatomy and embryology of the bridging and emissary veins were identified using one electronic database, supplemented by data from selected reference texts. Persisting fetal pial-arachnoidal veins correspond to the adult bridging veins. Relevant embryologic descriptions are based on the classic scheme of five divisions of the brain (telencephalon, diencephalon, mesencephalon, metencephalon, myelencephalon). Variation in their exact position and the number of bridging veins is the rule and certain locations, particularly that of the anterior cranial fossa and lower posterior cranial fossa are often neglected in prior descriptions. The distal segment of a bridging vein is part of the dural system and can be primarily involved in cranial dural arteriovenous lesions by constituting the actual site of the shunt. The veins in the lamina cribriformis exhibit a bridging-emissary vein pattern similar to the spinal configuration. The emissary veins connect the dural venous system with the extracranial venous system and are often involved in dural arteriovenous lesions. Cranial dural shunts may develop in three distinct areas of the cranial venous system: the dural sinuses and their interfaces with bridging veins and emissary veins. The exact site of the lesion may dictate the arterial feeders and original venous drainage pattern.






Similar content being viewed by others
References
Duvernoy HM (1975) The superficial veins of the human brain: veins of the brain stem and of the base of the brain. Springer, Berlin
Duvernoy H (1999) Human brain stem vessels, 2nd edn. Springer, Germany
Streeter G (1918) The developmental alterations in the vascular system of the brain of the human embryo. Contrib Embryol 271(24):5–38
Markowski J (1911) Uber die Entwicklung der Sinus durae matris und der Hirnvenen bei menschlichen Embryonen 15.5–49 mm. Bulletin de l’Academie des Sciences de Cracovie Serie B:590–611 [in German]
Padget D (1956) The cranial venous system in man in reference to development, adult configuration, and relation to the arteries. Am J Anat 98:307–355
Padget D (1957) The development of the cranial venous system in man from the viewpoint of comparative anatomy. Contrib Embryol 247:81–140
Dagain A (2008) Junction between the great cerebral vein and the straight sinus: an anatomical, immunohistochemical and ultrastructural study on 25 human brain cadaveric dissections. Clin Anat 21:389–397
Dagain A, Vignes R, Dulou R, Delmas JM, Riem T, Guerin J, Liguoro D (2009) Study of the junction between the cortical bridging veins and basal cranial venous sinus. Neurochirurgie 55(1):19–24. doi:10.1016/j.neuchi.2008.10.011
Han H, Tao W, Zhang M (2007) The dural entrance of cerebral bridging veins into the superior sagittal sinus: an anatomical comparison between cadavers and digital subtraction angiography. Neuroradiology 49(2):169–175. doi:10.1007/s00234-006-0175-z
Vignes JR, Dagain A, Guerin J, Liguoro D (2007) A hypothesis of cerebral venous system regulation based on a study of the junction between the cortical bridging veins and the superior sagittal sinus. laboratory investigation. J Neurosurg 107(6):1205–1210. doi:10.3171/JNS-07/12/1205
Lowenhielm P (1978) Tolerance level for bridging vein disruption calculated with a mathematical model. J Bioeng 2(6):501–507
Yamashima T, Friede RL (1984) Why do bridging veins rupture into the virtual subdural space? J Neurol Neurosurg Psychiatry 47(2):121–127
Maxeiner H (2001) Demonstration and interpretation of bridging vein ruptures in cases of infantile subdural bleedings. J Forensic Sci 46(1):85–93
Depreitere B, Van Lierde C, Sloten JV, Van Audekercke R, Van der Perre G, Plets C, Goffin J (2006) Mechanics of acute subdural hematomas resulting from bridging vein rupture. J Neurosurg 104(6):950–956. doi:10.3171/jns.2006.104.6.950
Maxeiner H (2001) Lethal subdural bleedings of babies–accident or abuse? Med Law 20(3):463–482
Vorkapic P, Perneczky A, Tschabitscher M, Knosp E, Flohr A (1985) Transsylvian approach to the tentorial hiatus—anatomical remarks on the microsurgical exposure. Zentralbl Neurochir 46(1):2–10
Kasama A, Kanno T (1989) A pitfall in the interhemispheric translamina terminalis approach for the removal of a craniopharyngioma. Significance of preserving draining veins. part II. Experiment Study Surg Neurol 32(2):116–120
Sakaki T, Kakizaki T, Takeshima T, Miyamoto K, Tsujimoto S (1995) Importance of prevention of intravenous thrombosis and preservation of the venous collateral flow in bridging vein injury during surgery: an experimental study. Surg Neurol 44(2):158–162
Sampei T, Yasui N, Okudera T, Fukasawa H (1996) Anatomic study of anterior frontal cortical bridging veins with special reference to the frontopolar vein. Neurosurgery 38(5):971–975
Ueyama T, Al-Mefty O, Tamaki N (1998) Bridging veins on the tentorial surface of the cerebellum: a microsurgical anatomic study and operative considerations. Neurosurgery 43(5):1137–1145
Kyoshima K, Oikawa S, Kobayashi S (2001) Preservation of large bridging veins of the cranial base: technical note. Neurosurgery 48(2):447–449
Kubota M, Saeki N, Yamaura A, Ono J, Ozawa Y (2001) Influences of venous involvement on postoperative brain damage following the anterior interhemispheric approach. Acta Neurochir (Wien) 143(4):321–325, discussion 325-326
Kaminogo M, Hayashi H, Ishimaru H, Morikawa M, Kitagawa N, Matsuo Y, Hayashi K, Yoshioka T, Shibata S (2002) Depicting cerebral veins by three-dimensional CT angiography before surgical clipping of aneurysms. AJNR Am J Neuroradiol 23(1):85–91
Kazumata K, Kamiyama H, Ishikawa T, Takizawa K, Maeda T, Makino K, Gotoh S (2003) Operative anatomy and classification of the sylvian veins for the distal transsylvian approach. Neurol Med Chir (Tokyo) 43(9):427–433. doi:JST.JSTAGE/nmc/43.427
Han H, Yao Z, Wang H, Deng X, Yu Fong AH, Zhang M (2008) Dural entrance of the bridging vein into the transverse sinus provides a reliable measure for preoperative planning: an anatomic comparison between cadavers and neuroimages. Neurosurgery 62(5 Suppl 2):ONS289–295. doi:10.1227/01.neu.0000326009.46197.ab
Davidson L, Krieger MD, McComb JG (2011) Posterior interhemispheric retrocallosal approach to pineal region and posterior fossa lesions in a pediatric population. J Neurosurg Pediatr 7(5):527–533. doi:10.3171/2011.2.PEDS10123
Gu SX, Yang DL, Cui DM, Xu QW, Che XM, Wu JS, Li WS (2011) Anatomical studies on the temporal bridging veins with Dextroscope and its application in tumor surgery across the middle and posterior fossa. Clin Neurol Neurosurg 113(10):889–894. doi:10.1016/j.clineuro.2011.06.008
Miyachi S, Izumi T, Matsubara N, Naito T, Haraguchi K, Wakabayashi T (2011) Mechanism of the formation of dural arteriovenous fistula: the role of the emissary vein. Interv Neuroradiol 17(2):195–202
Okudera T, Huang YP, Ohta T, Yokota A, Nakamura Y, Maehara F, Utsunomiya H, Uemura K, Fukasawa H (1994) Development of posterior fossa dural sinuses, emissary veins, and jugular bulb: morphological and radiologic study. AJNR Am J Neuroradiol 15(10):1871–1883
Rhoton AL Jr (2002) The cerebral veins. Neurosurgery 51(4 Suppl):S159–S205
Rhoton AL Jr (2000) The posterior fossa veins. Neurosurgery 47(3 Suppl):S69–S92
Lasjaunias P, Berenstein, A., ter Brugge, K. (2001) Surgical neuroangiography: clinical vascular anatomy and variations, vol 1. 2nd edn. Springer, Berlin Heidelberg
Mall FP (1905) On the development of the blood-vessels of the brain in the human embryo. Am J Anatomy 4(1):1–18. doi:10.1002/aja.1000040102
Miquel MA MJ, Cusi V, Naidich TP (1996) Embryogenesis of the veins of the posterior fossa: an overview. In: As H (ed) Surgery of intracranial venous system. Springer, Berlin Heidelberg, pp 14–25
Chen J, Wang XM, Luan LM, Chao BT, Pang B, Song H, Pang Q (2012) Biological characteristics of the cerebral venous system and its hemodynamic response to intracranial hypertension. Chin Med J (Engl) 125(7):1303–1309
Han H, Deng X, Fong AH, Zhang M (2010) Dural entrance of the bridging vein in the middle cranial fossa: a novel classification of the cerebral veins for preoperative planning. Neurosurgery 67(3 Suppl Operative):ons9-15. doi:10.1227/01.NEU.0000381683.27324.14
San Millan Ruiz D, Fasel JH, Rufenacht DA, Gailloud P (2004) The sphenoparietal sinus of breschet: does it exist? an anatomic study. AJNR Am J Neuroradiol 25(1):112–120
Tubbs RS, Salter EG, Wellons JC, Blount JP, Oakes WJ (2007) The sphenoparietal sinus. Neurosurgery 60(2 Suppl 1):ONS9–ONS12. doi:10.1227/01.neu.0000249241.35731.c6, discussion ONS12
Takahashi S, Sakuma I, Otani T, Yasuda K, Tomura N, Watarai J, Yanagisawa T, Mizoi K (2007) Venous anatomy of the sphenoparietal sinus: evaluation by MR imaging. Interv Neuroradiol 13(Suppl 1):84–89
Mortazavi MM, Denning M, Yalcin B, Shoja MM, Loukas M, Tubbs RS (2013) The intracranial bridging veins: a comprehensive review of their history, anatomy, histology, pathology, and neurosurgical implications. Child’s Nervous System ChNS. doi:10.1007/s00381-013-2054-3
Perese DM (1960) Superficial veins of the brain from a surgical point of view. J Neurosurg 17:402–412. doi:10.3171/jns.1960.17.3.0402
Gibbs E, Gibbs FA (1934) The cross section areas of the vessels that form the torcular and the manner in which flow is distributed to the right and to the left lateral sinus. Anat Rec 59:419–426
Krisht A, Barrow DL, Al-Mefty O, Dawson R, Shengelala G, Bonner G (1996) Venous anatomy of the vein of Labbé complex. In: As H (ed) Surgery of the intracranial venous system: embryology, anatomy, pathophysiology, neuroradiology, diagnosis, treatment. Springer, London, pp 36–42
Sakata K, Al-Mefty O, Yamamoto I (2000) Venous consideration in petrosal approach: microsurgical anatomy of the temporal bridging vein. Neurosurgery 47(1):153–160, discussion 160-151
Matsushima T, Suzuki SO, Fukui M, Rhoton AL Jr, de Oliveira E, Ono M (1989) Microsurgical anatomy of the tentorial sinuses. J Neurosurg 71(6):923–928. doi:10.3171/jns.1989.71.6.0923
Browder J, Kaplan HA (1976) Cerebral dural sinuses and their tributaries. American Lecture Series. C, Thomas
Tenchini (1905) Di un emissario anomalo dell’ orbito frontale. Monit Zool Ital Firenze anno xvi:(Abstract given in Schwalbe’s Jahresberichte für Anatomie, I905, P.990)
San Millán Ruíz DGP, Rüfenacht DA, Yilmaz H, Fasel JH (2006) Anomalous intracranial drainage of the nasal mucosa: a vein of the foramen caecum? AJNR Am J Neuroradiol 27(1):129–131
Cunningham DJ, Robinson, A. (1914) Cunningham’s Text-book of anatomy. W.Wood, New York
Standring S (2005) Gray’s anatomy: the anatomical basis of clinical practice, 39th edn. Elsevier Churchill Livingstone, New York
Onodi A (1910) The optic nerve and the accessory sinuses of the nose, a contribution to the study of canalicular neuritis and atrophy of the optic nerve of nasal origin. W.Wood, New York
Whitnall E (1921) The anatomy of the human orbit and accessory organs of vision. R.R. Clark, Edinburgh
Lang J (1981) Klinische Anatomie des Kopfes. Neurocranium, Orbita, kraniocervikaler Übergang. Springer, Berlin Heidelberg
Salamon G, Huang YP (1976) Radiologic anatomy of the brain. Springer, New York
Wolf BS, Huang YP, Newman CM (1963) The superficial sylvian venous drainage system. Am J Roentgenol Radium Therapy Nuclr Med 89:398–410
De Miquel MA, Mateu JMD, Cusi V, Naidich TP (1996) Embryogenesis of the veins of the posterior fossa: an overview. In: As H (ed) Surgery of the intracranial venous system: embryology, anatomy, pathophysiology, neuroradiology, diagnosis, treatment. Springer, London, pp 14–25
Tanriover N, Abe H, Rhoton AL Jr, Kawashima M, Sanus GZ, Akar Z (2007) Microsurgical anatomy of the superior petrosal venous complex: new classifications and implications for subtemporal transtentorial and retrosigmoid suprameatal approaches. J Neurosurg 106(6):1041–1050
Kiyosue H, Tanoue S, Sagara Y, Hori Y, Okahara M, Kashiwagi J, Nagatomi H, Mori H (2008) The anterior medullary-anterior pontomesencephalic venous system and its bridging veins communicating to the dural sinuses: normal anatomy and drainage routes from dural arteriovenous fistulas. Neuroradiology 50(12):1013–1023. doi:10.1007/s00234-008-0433-3
Matsushima T, Rhoton AL Jr, de Oliveira E, Peace D (1983) Microsurgical anatomy of the veins of the posterior fossa. J Neurosurg 59(1):63–105. doi:10.3171/jns.1983.59.1.0063
Baltsavias G, Bhatti A, Valavanis A (2013) Lateral convexial tributary sinus of superior sagittal sinus. a rare anatomic variation and the importance of its recognition. Clin Neurol Neurosurg 115(10):2268–2269. doi:10.1016/j.clineuro.2013.07.020
San Millan Ruiz D, Gailloud P, Rufenacht DA, Delavelle J, Henry F, Fasel JH (2002) The craniocervical venous system in relation to cerebral venous drainage. AJNR Am J Neuroradiol 23(9):1500–1508
Matsushima K, Kawashima M, Matsushima T, Hiraishi T, Noguchi T, Kuraoka A (2013) Posterior condylar canals and posterior condylar emissary veins-a microsurgical and CT anatomical study. Neurosurg Rev. doi:10.1007/s10143-013-0493-7
Schelling F (1978) The emissaries of the human skull (author’s transl). Anat Anz 143(4):340–382
Shane Tubbs R, Watanabe K, Loukas M, Cohen-Gadol AA (2013) Anatomy of the inferior petro-occipital vein and its relation to the base of the skull: application to surgical and endovascular procedures of the skull base. Clin Anat. doi:10.1002/ca.22268
Tubbs RS, Kelly DR, Humphrey ER, Chua GD, Shoja MM, Salter EG, Acakpo-Satchivi L, Wellons JC 3rd, Blount JP, Oakes WJ (2007) The tectorial membrane: anatomical, biomechanical, and histological analysis. Clin Anat 20(4):382–386. doi:10.1002/ca.20334
Coppini L, Sciascia R, Rondanelli E (1963) The communications between the intracranial and extracranial venous circulation by means of the emissary canals of the frontal bone. Bullet Delle Sci Med 135:238–266
Mortazavi MM, Tubbs RS, Riech S, Verma K, Shoja MM, Zurada A, Benninger B, Loukas M, Cohen Gadol AA (2012) Anatomy and pathology of the cranial emissary veins: a review with surgical implications. Neurosurgery 70(5):1312–1318. doi:10.1227/NEU.0b013e31824388f8, discussion 1318-1319
Lasjaunias P, Berenstein, A., ter Brugge, K. (2001) Surgical neuroangiography: dural arteriovenous shunts, vol 2.2. Springer, Berlin Heidelberg
Geibprasert S, Pereira V, Krings T, Jiarakongmun P, Toulgoat F, Pongpech S, Lasjaunias P (2008) Dural arteriovenous shunts: a new classification of craniospinal epidural venous anatomical bases and clinical correlations. Stroke 39(10):2783–2794. doi:10.1161/strokeaha.108.516757
Capra N, Anderson, K. (1984) Anatomy of the cerebral venous system. In: Kapp J, Schmidek, H. (eds) The cerebral venous system and its disorders. Grune & Stratton, New York, p 25
Piffer CR, Horn Y, Hureau J, Meininger V (1986) Anatomo-microscopic study of the walls of the superior cerebral veins. Anat Anz 162(5):331–350
Velut S, Santini JJ (1987) Microsurgical anatomy of the ampulla of Galen. Neurochirurgie 33(4):264–271
Ruchoux MM, Renjard L, Monegier du Sorbier C, Raybaud C, Santini JJ, Lhuintre Y (1987) Histopathology of the vein of Galen. Neurochirurgie 33(4):272–284
Dagain A, Vignes JR, Dulou R, Dutertre G, Delmas JM, Guerin J, Liguoro D (2008) Junction between the great cerebral vein and the straight sinus: an anatomical, immunohistochemical, and ultrastructural study on 25 human brain cadaveric dissections. Clin Anat 21(5):389–397. doi:10.1002/ca.20635
Bailey P (1948) Intracranial tumors, 2nd edition. Charles C. Thomas, Springfield, IL, USA
Mitsuhashi Y, Aurboonyawat T, Pereira VM, Geibprasert S, Toulgoat F, Ozanne A, Lasjaunias P (2009) Dural arteriovenous fistulas draining into the petrosal vein or bridging vein of the medulla: possible homologs of spinal dural arteriovenous fistulas. CLINICAL article. J Neurosurg 111(5):889–899. doi:10.3171/2009.1.JNS08840
Piske RL, Lasjaunias P (1988) Extrasinusal dural arteriovenous malformations. report of three cases. Neuroradiology 30(5):426–432
MlF O’RR (1999) The embryonic human brain. an atlas of developmental stages, 2nd edn. Wiley, New York
Puelles L, Harrison M, Paxinos G, Watson C (2013) A developmental ontology for the mammalian brain based on the prosomeric model. Trends Neurosci 36(10):570–8. doi:10.1016/j.tins.2013.06.004
Puelles L, Ferran JL (2012) Concept of neural genoarchitecture and its genomic fundament. Front Neuroanat 6:47. doi:10.3389/fnana.2012.00047
Shimamura K, Hartigan DJ, Martinez S, Puelles L, Rubenstein JL (1995) Longitudinal organization of the anterior neural plate and neural tube. Development (Cambridge, England) 121(12):3923–3933
Rubenstein JL, Martinez S, Shimamura K, Puelles L (1994) The embryonic vertebrate forebrain: the prosomeric model. Science (New York, NY) 266(5185):578–580
Hofmann M (1901) Zur vergleichenden Anatomie der Gehirn- und Rückenmarksarterien der Vertebraten. Z Morphol Anthropol 2:248–322
Sterzi G (1904) Die Blutgefäße des Rückenmarks. untersuchungen über ihre vergleichende anatomie und entwicklungsgeschichte. Anat H 74:1–364
Ernst R, Bulas R, Tomsick T, van Loveren H, Aziz KA (1999) Three cases of dural arteriovenous fistula of the anterior condylar vein within the hypoglossal canal. AJNR Am J Neuroradiol 20(10):2016–2020
Abiko M, Ikawa F, Ohbayashi N, Mitsuhara T, Ichinose N, Inagawa T (2008) Endovascular treatment for dural arteriovenous fistula of the anterior condylar confluence involving the anterior condylar vein. a report of two cases. Interv Neuroradiol 14(3):313–317
Miyachi S, Ohshima T, Izumi T, Kojima T, Yoshida J (2008) Dural arteriovenous fistula at the anterior condylar confluence. Interv Neuroradiol 14(3):303–311
Choi JW, Kim BM, Kim DJ, Kim DI, Suh SH, Shin NY, Lee JG (2013) Hypoglossal canal dural arteriovenous fistula: incidence and the relationship between symptoms and drainage pattern. J Neurosurg 119(4):955–960. doi:10.3171/2013.4.jns121974
Park JY, Ahn JY, Lee BH, Huh R, Choi HK, Shin MS (2001) Therapeutic embolization of the dural arteriovenous malformation involving the jugular bulb. J Korean Med Sci 16(4):527–531
Okahara M, Kiyosue H, Tanoue S, Sagara Y, Hori Y, Kashiwagi J, Mori H (2007) Selective transvenous embolization of dural arteriovenous fistulas involving the hypoglossal canal. Interv Neuroradiol 13(1):59–66
Tirakotai W, Benes L, Kappus C, Sure U, Farhoud A, Bien S, Bertalanffy H (2007) Surgical management of dural arteriovenous fistulas with transosseous arterial feeders involving the jugular bulb. Neurosurg Rev 30(1):40–48. doi:10.1007/s10143-006-0056-2, discussion 48-49
Manabe S, Satoh K, Matsubara S, Satomi J, Hanaoka M, Nagahiro S (2008) Characteristics, diagnosis and treatment of hypoglossal canal dural arteriovenous fistula: report of nine cases. Neuroradiology 50(8):715–721. doi:10.1007/s00234-008-0393-7
Byun JS, Hwang SN, Park SW, Nam TK (2009) Dural arteriovenous fistula of jugular foramen with subarachnoid hemorrhage : selective transarterial embolization. J Korean Neurosurg Soc 45(3):199–202. doi:10.3340/jkns.2009.45.3.199
Borden JA, Wu JK, Shucart WA (1995) A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg 82(2):166–179. doi:10.3171/jns.1995.82.2.0166
Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A, Chiras J, Merland JJ (1995) Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology 194(3):671–680
Boyd GI (1930) The emissary foramina of the cranium in man and the anthropoids. J Anat 65(Pt 1):108–121
Inoue A, Tagawa M, Kumon Y, Watanabe H, Shoda D, Sugiu K, Ohnishi T (2014) Ethmoidal dural arteriovenous fistula with unusual drainage route treated by transarterial embolization. J Neurointerventional Surg. doi:10.1136/neurintsurg-2013-011098.rep
Acknowledgments
We wish to thank Professor V. Runge for his valuable comments on the manuscript and knowledgeable suggestions.
Conflict of interest
We declare that we have no conflict of interest.
Financial support
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Timo Krings, Toronto, Canada
It is common knowledge that the more sophisticated a classification, the better its predictive value, but the more complicated will be its applicability in everyday clinical care. The classification of dural AVF is a good example for this: The Toronto group proposed the most simplistic (and therefore easy to use) type of classification: “benign” dAVF have no cortical venous reflux, drain toward the heart, and have a good clinical prognosis, whereas “malignant” dAVF demonstrate cortical venous reflux and present with a high risk of hemorrhage and neurologic deficits [1, 2]. From the dichotomic classification, Borden moved on to further classify the malignant dAVF into those that had the reflux through a venous sinus and those that refluxed immedialtey into pial veins [3]. Given the large variability seen in patients with dAVF, it soon became obvious that more groups may even better subclassify these lesions and the Cognard classification had seven distinct subtypes [4].
While these classifications were mainly based upon analysis of the venous drainage assuming that all dAVF constitute the same type of disease, the Bicetre group challenged this assumption based on the finding that certain dAVF had a striking gender predilection [5, 6]. Their classification proposed that the primary role of the vein that is initially affected by the shunt will determine whether or not reflux will occur: If so, role of the affected vein was, to drain the brain, reflux will be present (and interestingly these dAVF had a significant male predilection) whereas those veins that are primarily involved into drainage of the bone will only present with cortical venous reflux if additional (secondary) outflow restrictions are present downstream from the shunt. While this classification helps to understand dAVF and their drainage pattern, it did not add to our treatment decision-making process.
The present classification represents an amalgamation of the different classification systems thus attempting to not only predict reflux but also to better predict clinical presentation and thus guiding our treatment decisions. It is based on the significant experience with and the deep understanding of dural arteriovenous fistulas of the senior author, Prof. Valavanis, who over the course of the past 19 years treated endovascularly the majority of the 211 patients with dAVF reported in this paper, and whose clinical and angiographical data were retrospectively reviewed and meticulously analyzed by the lead author, Dr. Baltsavias who treated several of the patients since 2009 and has to be commended for this major undertaking and for furthering our understanding of dAVF.
In the first part of the manuscript, Dr. Baltsavias introduces the concept of bridging and emissary veins and how they relate to the epidural spaces: While the bridging vein interconnect the pial veins with the dural sinuses, the emissary veins will interconnect the dural sinuses with the extracranial venous system thus being transitory conduits on opposite “borders” of the dural sinuses. The bridging veins represent pial-arachnoidal-dural connectors and are in their distal veno-sinusal junction related to the dural sinuses, i.e., they represent the lateral epidural spaces as proposed by the Bicetre classification. Given their location, shunts into these veins will invariably lead to cortical venous reflux.
The emissary veins on the other hand represent the connection of the dural sinuses to the extradural venous vessels and thus include the jugular bulbs, as well as the cavernous sinus. Shunts at these sites are expected to recuit osteodural feeder and are similar to the “ventral epidural spaces” of the Bicetre classification being primarily involved in drainage of the bone and leading primarily not to cortical venous reflux. The site of the shunt will thus not only dictate the venous drainage pattern but also the type of arterial feeder.
In the second part, the relation between the bridging veins and the leptomeningeal drainage is further evaluated highlighting the presence of thrombotic phenomena in the vast majority of cranial dAVF with purely leptomeningeal drainage. Dr. Baltsavias described three different patterns that can be encountered: a dural AVF engaging a bridging vein with occlusion of the veno-dural transition, a dural AVF into an isolated sinus, and a dural AVF into the veins close to the cribriforme plate.
Within the third part of this work, a revised classification of dAVF is proposed based on a detailed analysis of the angioarchitecture according to three factors: directness of venous drainage (depending on the location of the shunt), exclusiveness of the pial venous drainage (related to venous outflow obstruction), and venous strain (as evidenced by venous congestion or venous ectasias). These factors will lead to eight different subtypes of dural AVF and may be better suited to identify which patients present with aggressive clinical symptoms, which ultimately will benefit the patient by identifying patients at risk.
Finally, in the fourth part of this series, the thus developed classification scheme is tested in the series of the authors, and indeed, they were able to demonstrate that directness, exclusivity and signs for venous decompensation could better predict clinical outcome as compared to the simplistic classification of “benign” and “malignant” shunts.
This classification scheme will help to identify high-risk patients, and the authors have to be commended for their thorough and concise analysis of one of the largest series of dAVF managed at a single institution.
References
1. Davies MA, TerBrugge K, Willinsky R, Coyne T, Saleh J, Wallace MC. The validity of classification for the clinical presentation of intracranial dural arteriovenous fistulas. J Neurosurg. 1996 Nov;85(5):830–7
2. van Dijk JM, terBrugge KG, Willinsky RA, Wallace MC. Clinical course of cranial dural arteriovenous fistulas with long-term persistent cortical venous reflux. Stroke. 2002 May;33(5):1233–6
3. Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg. 1995 Feb;82(2):166–79.
4. Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A, Chiras J, Merland JJ. Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995 Mar;194(3):671–80
5. Geibprasert S, Pereira V, Krings T, Jiarakongmun P, Toulgoat F, Pongpech S, Lasjaunias P. Dural arteriovenous shunts: a new classification of craniospinal epidural venous anatomical bases and clinical correlations. Stroke. 2008 Oct;39(10):2783-94.
6. Geibprasert S, Krings T, Pereira V, Pongpech S, Piske R, Lasjaunias P. Clinical characteristics of dural arteriovenous shunts in 446 patients of three different ethnicities. Interv Neuroradiol. 2009 Dec;15(4):395–400.
Michihiro Tanaka, Kamogawa City, Japan
The authors summarize the embryological aspect of the regional bridging and emissary veins based on a systematic review of the literature. They use the nomenclature in a strict way, paying special attention to the difference between bridging and emissary vein in terms of embryological aspect. This approach is quite unique and helps us to understand the functional anatomy of the venous drainage system of the brain and cranium.
Karel terBrugge, Toronto, Canada
Dr. Baltsavias and the Zurich team are to be congratulated on this in-depth review of the intracranial venous vascular anatomy as it pertains to the relationships of the pial venous system draining toward the dural sinuses via the bridging venous system and the emissary veins representing the communication between the dural sinuses and the extracranial venous system except for at the anterior cranial fossa level where this may not occur due to the local absence of a dural sinus and the potential drainage via “bridging” leptomeningeal anastomoses connecting the adjacent pial venous system with the extracranial venous system at the level of the nasal fossa. This explains clearly the fact that patients with brain AVMs may present with nose bleeds and patients with cribriforme plate dural shunts may present with either epistaxis or intracranial hemorrhage.
Rights and permissions
About this article
Cite this article
Baltsavias, G., Parthasarathi, V., Aydin, E. et al. Cranial dural arteriovenous shunts. Part 1. Anatomy and embryology of the bridging and emissary veins. Neurosurg Rev 38, 253–264 (2015). https://doi.org/10.1007/s10143-014-0590-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-014-0590-2