Abstract
Purpose
In this study, the potential of semiquantitative and quantitative analysis of dynamic contrast-enhanced (DCE) magnetic resonance imaging (MRI) was investigated to differentiate glioblastoma (GB) from radiation necrosis (RN) in rats.
Procedures
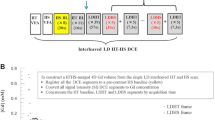
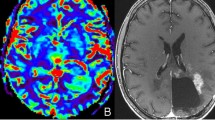
F98 GB growth was seen on MRI 8–23 days post-inoculation (n = 15). RN lesions developed 6–8 months post-irradiation (n = 10). DCE-MRI was acquired using a fast low-angle shot (FLASH) sequence. Regions of interest (ROIs) encompassed peripheral contrast enhancement in GB (n = 15) and RN (n = 10) as well as central necrosis within these lesions (GB (n = 4), RN (n = 3)). Dynamic contrast-enhanced time series, obtained from the DCE-MRI data, were fitted to determine four function variables (amplitude A, offset from zero C, wash-in rate k, and wash-out rate D) as well as maximal intensity (ImaxF) and time to peak (TTPF). Secondly, maps of semiquantitative and quantitative parameters (extended Tofts model) were created using Olea Sphere (O). Semiquantitative DCE-MRI parameters included wash-inO, wash-outO, area under the curve (AUCO), maximal intensity (ImaxO), and time to peak (TTPO). Quantitative parameters included the rate constant plasma to extravascular-extracellular space (EES) (K trans), the rate constant EES to plasma (K ep), plasma volume (V p), and EES volume (V e). All (semi)quantitative parameters were compared between GB and RN using the Mann-Whitney U test. ROC analysis was performed.
Results
Wash-in rate (k) and wash-out rate (D) were significantly higher in GB compared to RN using curve fitting (p = 0.016 and p = 0.014). TTPF and TTPO were significantly lower in GB compared to RN (p = 0.001 and p = 0.005, respectively). The highest sensitivity (87 %) and specificity (80 %) were obtained for TTPF by applying a threshold of 581 s. K trans, K ep, and V e were not significantly different between GB and RN. A trend towards higher V p values was found in GB compared to RN, indicating angiogenesis in GB (p = 0.075).
Conclusions
Based on our results, in a rat model of GB and RN, wash-in rate, wash-out rate, and the time to peak extracted from DCE-MRI time series data may be useful to discriminate GB from RN.






Similar content being viewed by others
References
Ahmed R, Oborski MJ, Hwang M et al (2014) Malignant gliomas: current perspectives in diagnosis, treatment, and early response assessment using advanced quantitative imaging methods. Cancer Manag Res 6:149–170
Stupp R, Dietrich PY, Ostermann Kraljevic S et al (2002) Promising survival for patients with newly diagnosed glioblastoma multiforme treated with concomitant radiation plus temozolomide followed by adjuvant temozolomide. J Clin Oncol 20:1375–1382
Brandsma D, Stalpers L, Taal W et al (2008) Clinical features, mechanisms, and management of pseudoprogression in malignant gliomas. Lancet Oncol 9:453–461
Siu A, Wind JJ, Iorgulescu JB et al (2012) Radiation necrosis following treatment of high grade glioma-a review of the literature and current understanding. Acta Neurochir 154:191–201
Wen PY, Macdonald DR, Reardon DA et al (2010) Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol 28:1963–1972
Bobek-Billewicz B, Stasik-Pres G, Majchrzak H et al (2010) Differentiation between brain tumor recurrence and radiation injury using perfusion, diffusion-weighted imaging and MR spectroscopy. Folia Neuropathol 48:81–92
Alexiou GA, Tsiouris S, Kyritsis AP et al (2009) Glioma recurrence versus radiation necrosis: accuracy of current imaging modalities. J Neuro-Oncol 95:1–11
Hustinx R, Pourdehnad M, Kaschten B et al (2005) PET imaging for differentiating recurrent brain tumor from radiation necrosis. Radiol Clin N Am 43:35–47
Zhou J, Tryggestad E, Wen Z et al (2011) Differentiation between glioma and radiation necrosis using molecular resonance imaging of endogeneous proteins and peptides. Nat Med 17:130–134
Wang S, Chen Y, Lal B et al (2012) Evaluation of radiation necrosis and malignant glioma in rat models using diffusion tensor MR imaging. J Neuro-Oncol 107:51–60
Mullins ME, Barest GD, Schaefer PW et al (2005) Radiation necrosis versus glioma recurrence: conventional MR imaging clues to diagnosis. Am J Neuroradiol 26:1967–1972
Spaeth N, Wyss MT, Weber B et al (2004) Uptake of 18F-fluorocholine, 18F-fluoroethyl-L-tyrosine, and 18F-FDG in acute cerebral radiation injury in the rat: implications for separation of radiation necrosis from tumor recurrence. J Nucl Med 45:1931–1938
Van Laere K, Ceyssens S, Van Calenbergh F et al (2005) Direct comparison of 18F-FDG and 11C-methionine PET in suspected recurrence of glioma: sensitivity, inter-observer variability and prognostic value. Eur J Nucl Med Mol Imaging 32:39–51
Chao ST, Suh JH, Raja S et al (2001) The sensitivity and specificity of FDG PET in distinguishing recurrent brain tumor from radionecrosis in patients treated with stereotactic radiosurgery. Int J Cancer 96:191–197
Bolcaen J, Descamps B, Deblaere K et al (2015) 18F-fluoromethylcholine (FCho), 18F-fluoroethyltyrosine (FET), and 18F-fluorodeoxyglucose (FDG) for the discrimination between high-grade glioma and radiation necrosis in rats: a PET study. Nucl Med and Biol 42:38–45
Minamimoto R, Saginoya T, Kondo C et al (2015) Differentiation of brain tumor recurrence from post-radiotherapy necrosis with [11C]methionine PET: visual assessment versus quantitative assessment. PLoS One 10:e0132515
Galldiks N, Stoffels G, Filss CP et al (2012) Role of O-(2-18F-fluoroethyl)-L-tyrosine PET for differentiation of local recurrent brain metastasis from radiation necrosis. J Nucl Med 53:1367–1374
Karunanithi S, Sharma P, Kumar A et al (2013) 18F-FDOPA PET/CT for detection of recurrence in patients with glioma: prospective comparison with 18F-FDG PET/CT. Eur J Nucl Med Mol Imaging 40:1025–1035
Jena A, Taneja S, Gambhir A et al (2016) Glioma recurrence versus radiation necrosis single-session multiparametric approach using simultaneous O-(2-18F-fluoroethyl)-L-tyrosine PET/MRI. Clin Nucl Med 41:e228–e236
Mehrkens JH, Pöpperl G, Rachinger W et al (2008) The positive predictive value of 0-(2-(18F)fluoroethyl)-L-tyrosine (FET) PET in the diagnosis of a glioma recurrence after multimodal treatment. J Neuro-Oncol 88:27–35
Pöpperl G, Götz C, Rachinger W et al (2006) Serial 0-(2-(18F)fluoroethyl)-L-tyrosine PET for monitoring the effects of intracavitary radioimmunotherapy in patients with malignant glioma. Eur J Nucl Med Mol Imaging 33:792–800
Doyle WK, Budinger TF, Valk PE et al (1987) Differentiation of cerebral radiation necrosis from tumor recurrence by [18F]FDG and 82Rb positron emission tomography. J Comput Assist Tomogr 11:563–570
Kahn D, Follett KA, Bushnell DL et al (1994) Diagnosis of recurrent brain tumor: value of 201T1 SPECT vs 18F-fluorodeoxyglucose PET. Am J Roentgenol 163:1459–1465
Ricci PE, Karis JP, Heiserman JE et al (1998) Differentiating recurrent tumor from radiation necrosis: time for re-evaluation of positron emission tomography? Am J Neuroradiol 19:407–413
Kim YH, Oh SW, Lim YJ et al (2010) Differentiating radiation necrosis from tumor recurrence in high-grade gliomas: assessing the efficacy of 18F-FDG PET, 11C-methionine PET and perfusion MRI. Clin Neurol Neurosurg 112:758–765
Shah A, Snelling B, Bregy A et al (2013) Discriminating radiation necrosis from tumor progression in gliomas: a systematic review what is the best imaging modality? J Neuro-Oncol 112:141–152
Zeng QS, Li CF, Liu H et al (2007) Distinction between recurrent glioma and radiation injury using magnetic resonance spectroscopy in combination with diffusion-weighted imaging. Int J Radiation Oncology Biol Phys 68:151–158
Kim HS, Goh MJ, Kim N et al (2014) Which combination of MR imaging modalities is best for predicting recurrent glioblastoma? Study of diagnostic accuracy and reproducibility. Radiology 273:831–843
Hu LS, Baxter LC, Smith KA et al (2009) Relative cerebral blood volume values to differentiate high-grade glioma recurrence from posttreatment radiation effect: direct correlation between image-guided tissue histopathology and localized dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging measurements. Am J Neuroradiol 30:552–558
Barajas RF Jr, Chang JS, Segal MR et al (2009) Differentiation of recurrent glioblastoma multiforme from radiation necrosis after external beam radiation therapy with dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging. Radiology 253:486–496
Zahra MA, Tan LT, Priest AN et al (2009) Semiquantitative and quantitative dynamic contrast-enhanced magnetic resonance imaging measurements predict radiation response in cervix cancer. Int J Radiation Oncology Biol Phys 74:776–773
Bisdas S, Naegele T, Ritz R et al (2011) Distinguishing recurrent high-grade gliomas from radiation injury: a pilot study using dynamic contrast-enhanced MR imaging. Acad Radiol 18:575–583
Larsen VA, Simonsen HJ, Law I et al (2013) Evaluation of dynamic contrast-enhanced T1-weighted perfusion MRI in the differentiation of tumor recurrence from radiation necrosis. Neuroradiology 55:361–369
Narang J, Jain R, Arbab AS et al (2011) Differentiating treatment-induced necrosis from recurrent/progressive brain tumor using nonmodel-based semiquantitative indices derived from dynamic contrast-enhanced T1-weighted MR perfusion. Neuro-Oncology 13:1037–1046
Artzi M, Liberman G, Nadav G et al (2016) Differentiation between treatment-related changes and progressive disease in patients with high grade brain tumors using support vector machine classification based on DCE MRI. J Neuro-Oncol 127:515–524
Thomas AA, Arevalo-Perez J, Kaley T et al (2015) Dynamic contrast enhanced T1 MRI perfusion differentiates pseudoprogression from recurrent glioblastoma. J Neuro-Oncol 125:183–190
Barth RF, Kaur B (2009) Rat brain tumor models in experimental neuro-oncology: the C6, 9L, T9, RG2, F98, BT4C, RT-2 and CNS-1 gliomas. J Neuro-Oncol 94:299–312
Bolcaen J, Descamps B, Deblaere K et al (2014) MRI-guided 3D conformal arc micro-irradiation of a F98 glioblastoma rat model using the Small Animal Radiation Research Platform (SARRP). J Neuro-Oncol 120:257–266
Lemasson B, Serduc R, Maisin C et al (2010) Monitoring blood-brain barrier status in a rat model of glioma receiving therapy: dual injection of low-molecular-weight and macromolecular MR contrast media. Radiology 257:342–352
Padhani AR, Husband JE (2001) Dynamic contrast-enhanced MRI studies in oncology with an emphasis on quantification, validation and human studies. Clin Radiol 56:607–620
Jain R, Narang J, Sundgren PM et al (2010) Treatment induced necrosis versus recurrent/progressing brain tumor: going beyond the boundaries of conventional morphologic imaging. J Neuro-Oncol 100:17–29
Stapleton S, Jaffray D, Milosevc M (2016) Radiation effects on the tumor microenvironment: implications for nanomedicine delivery. Adv Drug Deliver Rev doi:10.1016/j.addr.2016.05.021
Li SP, Padhani AR (2012) Tumor response assessments with diffusion and perfusion MRI. J Mag Reson Imag 35:745–763
Heye AK, Culling RD, Valdes Hernandez MC et al (2014) Assessment of blood-brain barrier disruption using dynamic contrast-enhanced MRI. A systematic review. NeuroImage Clin 6:262–274
Buckley DL (2002) Uncertainty in the analysis of tracer kinetics using dynamic contrast-enhanced T1-weighted MRI. Magn Reson Med 47:601–606
Acknowledgements
This work was supported by Stichting Luka Hemelaere (O.L. Vrouwstraat 40, 8500 Kortrijk, Belgium) and Soroptimist International (S.I.B vzw, Middaglijnstraat 10, 1210 Brussel, Belgium).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Ghent University ethics committee for animal experiments (ECD 12/28).
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Bolcaen, J., Descamps, B., Acou, M. et al. In Vivo DCE-MRI for the Discrimination Between Glioblastoma and Radiation Necrosis in Rats. Mol Imaging Biol 19, 857–866 (2017). https://doi.org/10.1007/s11307-017-1071-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11307-017-1071-0