Abstract
Zika virus (ZIKV) is a mosquito-borne arbovirus from the Flaviviridae family, first discovered in 1947. There has been no report of severe complications caused by this virus in humans until recently. However, it is confirmed now that prenatally acquired ZIKV infection may cause severe congenital brain abnormalities in the infected fetuses. In addition, there has been an increasing number of reports during recent years about the causal relationship between postnatally acquired ZIKV infection and severe neurologic complications (mostly immune-mediated ones). Hence, ZIKV should not be considered as benign as it was initially thought, but it might be seen as a serious global threat to human health that may severely affect not only fetuses. In this pictorial essay, we aim to describe and illustrate the currently recognized spectrum of neuroimaging findings in postnatally acquired ZIKV infection. Although neurologic complications do not frequently occur in postnatal ZIKV infection, it is important to be aware of them because they may cause high morbidity and mortality in the affected patients. In addition to clinical and laboratory findings, neuroimaging may help in the diagnostic work-up to make the correct diagnosis, determine the extent of the disease, and follow the clinical course.
Similar content being viewed by others
Introduction
Zika virus (ZIKV) is a mosquito-borne arbovirus from the Flaviviridae family, which was first detected in monkeys in 1947 in the Zika Forest, Uganda, Africa. Unlike some other flaviviruses, ZIKV was not initially considered as a major cause for neurologic diseases in humans. However, since the recent outbreak in French Polynesia in 2013 and the subsequent epidemic in Brazil and other South American and Caribbean countries in 2015, there have been several reports of ZIKV infected patients suffering from severe neurologic symptoms. In addition, it is confirmed now that prenatal ZIKV infection causes severe brain abnormalities in the infected fetuses (so-called congenital Zika syndrome). Therefore, ZIKV should not be considered as benign as it was initially thought, but it might be seen as a serious emerging global threat. It should be emphasized that when discussing neurological complications caused by Zika virus, it is extremely important to differentiate between prenatally acquired and postnatally acquired infection. Prenatal ZIKV infection is transmitted to the fetus vertically from the infected mother; whereas postnatal ZIKV infection is mostly transmitted by mosquito bite (Aedes aegypti as the main vector), although transmission via sexual contact, blood transfusion, and accidental inoculation are also possible [1,2,3,4].
Postnatally acquired ZIKV infection is asymptomatic or mildly symptomatic in the majority of infected patients. It has been estimated that only 20% of infected patients show mild symptoms such as fever, myalgia, arthralgia, maculopapular rash, and conjunctivitis. However, in a small number of patients, postnatal Zika infection may cause severe neurological complications including Guillain–Barré syndrome (GBS), acute transverse myelitis (ATM), meningoencephalitis, and acute disseminated encephalomyelitis (ADEM). Although ZIKV may primarily injure the neuronal cells in the fetuses, postnatal ZIKV-related acute neurological complications are most likely caused by neuronal damage and demyelination due to humoral and cellular inflammatory mediators [1,2,3,4,5]. History, clinical presentation, neurophysiology studies including electromyography (EMG) and nerve conduction study (NCS), as well as serology and molecular testing of blood, urine and/or cerebrospinal fluid such as Ig-M, Ig-G, and real-time reverse transcription polymerase chain reaction (rRT-PCR) for the virus ribonucleic acid (RNA) play a key role in the diagnosis of postnatal ZIKV-related neurological complications [4, 5]. Neuroimaging may help in the patient work-up to make the correct diagnosis, determine the extent of the disease, and follow the clinical course.
In this pictorial essay, we aim to describe and illustrate the currently recognized spectrum of neuroimaging findings in postnatally acquired ZIKV infection.
ZIKV–related Guillain–Barré syndrome (GBS)
There are several reports indicating a strong association between ZIKV infection and an increased number of GBS cases in the endemic areas. GBS is an acute immune-mediated polyneuropathy, which mainly affects the peripheral nervous system (including motor, sensory, and autonomic nerves). As a result, the patient suffers from rapidly progressive muscle weakness and disturbed sensation. The classic clinical findings include symmetrical ascending paralysis, areflexia/hyporeflexia, and mild to moderate sensory and/or autonomic dysfunction without an obvious sensory level. GBS is a neurological emergency with potentially high morbidity and mortality when respiratory insufficiency develops. The majority of GBS patients in the ZIKV endemic areas are males (67%), and most of them are younger than 50 years old (94%), particularly younger than 20 years old (70%). Nearly all ZIKV-related GBS patients experience a symptomatic infection. The mean duration between onset of ZIKV-related symptoms and GBS development is about 7 days, and near half of patients have persistent symptoms of ZIKV infection during this period. Presentations in most ZIKV-related GBS cases are compatible with the acute motor axonal neuropathy (AMAN) subtype, which is a pure motor neuropathy with mild loss of reflexes and usually shows rapid recovery [5,6,7,8].
Brain and particularly spine MRI is increasingly used in the diagnostic work-up of GBS (Fig. 1). The main aim is to rule out other causes of acute flaccid paralysis, such as transverse myelitis (another potential complication in ZIKV infection). The administration of gadolinium-based contrast agents is essential because non-contrast enhanced imaging may appear completely normal. On spine MRI, the most common findings include post-contrast enhancement of the conus medullaris and cauda equina nerve roots (most commonly seen in the anterior nerve roots). In addition, T2-hyperintensity and post-contrast enhancement of the lumbar spinal ganglia may be seen bilaterally. On brain MRI, cranial nerves may reveal post-contrast enhancement, especially facial (VII) and trigeminal (V) nerves in the order of decreasing frequency [5, 9, 10].
ZIKV–related Guillain–Barré syndrome associated with Bickerstaff’s brainstem encephalitis (encephaloradiculomyelitis). Brain and spine MRI of a 35-year-old Brazilian male with progressive ascending paralysis in the lower limbs, evolved to respiratory distress and decreased level of consciousness. The patient had skin rashes preceded by flu-like symptoms, 1 week prior to the development of neurologic symptoms. Cerebrospinal fluid analysis was suggestive of Zika virus infection. Axial T2-weighted brain image shows bilateral hyperintensity (arrow) in the middle cerebellar peduncles (a). Post-contrast enhancement is seen in the cauda equina nerve roots (arrows) on sagittal (b) and axial (d) T1-weighted spine images following gadolinium-based contrast agent injection. Axial T2-weighted spine image reveals hyperintensity (arrow) in the anterior horns of the thoracic spinal cord (c)
ZIKV–related acute transverse myelitis (ATM)
A few reports revealed an association between ZIKV infection and transverse myelitis in the infected adults, although the causal relationship has not been confirmed yet. ATM is a relatively rare immune-mediated disease, which is secondary to perivascular lymphocytic infiltration leading to demyelination in the spinal cord. Patients typically present with variable motor, sensory, and autonomic dysfunction depending on the location and extent of cord involvement. An important and distinctive finding in the physical examination is the presence of a sensory level [11, 12].
On spine MRI, the signal abnormality usually involves more than 3 segments of the spinal cord in length (best appreciated on the sagittal images), and greater than two thirds in surface-area (best appreciated on the axial images). The signal changes are best seen on fluid-sensitive pulse sequences [e.g., T2-weighted image, short-tau inversion recovery (STIR), and fluid-attenuated inversion recovery (FLAIR)] as hyperintense areas, and the spinal cord may be enlarged due to edema. Variable degrees and patterns of post-contrast enhancement may be present in the involved segments of the spinal cord [11, 12].
ZIKV–related meningoencephalitis
Meningoencephalitis is a well-known and common presentation of flavivirus infections such as Japanese encephalitis or West Nile fever. However, there are limited reports on the occurrence of meningoencephalitis due to ZIKV. Patients may present with fever, encephalopathy (e.g., altered mental status), seizure, headache and vomiting due to increased intracranial pressure, motor and sensory dysfunction, cranial nerve palsy, and nuchal rigidity [14, 15].
Due to paucity of data, no specific neuroimaging pattern has emerged so far for ZIKV-related meningoencephalitis. The limited data suggests that ZIKV may cause asymmetric subcortical hyperintense lesions that are best seen on fluid-sensitive pulse sequences. In addition, these lesions may show restricted diffusion, suggesting cytotoxic edema (Fig. 2) [14,15,16].
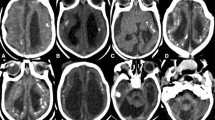
ZIKV-related meningoencephalitis. Brain MRI of an 81-year-old French male with fever, left-side hemiplegia, right upper limb paresis, and altered mental status, 10 days after returning from a cruise in New Caledonia, Vanuatu, Solomon Islands, and New Zealand. Blood and cerebrospinal fluid analyses were suggestive of Zika virus infection. Axial fluid-attenuated inversion recovery images (a, b) show hyperintense signal within the right perirolandic region (arrow in a), right occipital subcortical white matter (dashed arrow in b), and basal ganglia (short arrow in b) compatible with meningoencephalitis. Trace of diffusion images (c, d) reveal multiple punctuated bright foci (arrows) suggesting restricted diffusion, most likely secondary to cytotoxic edema and ischemic changes
A recent report of ZIKV-related encephalitis in an immunocompromised patient has suggested that, in contrast to encephalitis secondary to other flaviviruses (such as Japanese encephalitis, or West Nile virus), which typically and more commonly demonstrate hyperintensity in basal ganglia, thalami, brainstem, and cerebellum with relative cerebral cortical sparing on fluid-sensitive pulse sequences, ZIKV may have a predilection for cortical gray matter and subcortical white matter, particularly for the cingulate and superior frontal gyrus [15]. It should be emphasized that although not frequent, Japanese encephalitis and West Nile viruses may cause cortical lesions as well (usually in conjunction with the characteristic deep gray matter involvement) [17, 18]. On the other hand, there is a report of diffuse involvement of white matter and deep gray matter nuclei in a case of ZIKV-related encephalitis leading to death [16]. In addition, we present a case of ZIKV-related GBS associated with Bickerstaff’s brainstem encephalitis, in whom both cerebellar peduncles showed hyperintense lesions on fluid-sensitive pulse sequences (Fig. 1).
ZIKV–related acute disseminated encephalomyelitis (ADEM)
ADEM is an immune-mediated disorder that involves both brain and spinal cord white matter, resulting in variable degrees of demyelination. Gray matter (particularly the basal ganglia) is also typically involved. ADEM usually has a monophasic course characterized by fever, encephalopathy (e.g., decreased level of consciousness), seizures, headaches, motor and sensory deficits, and behavioral changes [5, 18].
On brain MRI, multiple ill-defined, asymmetric lesions involving the subcortical and deep white matter and deep gray matter nuclei are typically seen. The lesions have a hyperintense signal on fluid-sensitive sequences. Contrast enhancement is uncommon and, when present, is usually homogenous in all lesions. Diffusion restriction may be seen in the acute stage of the disease [5, 18].
Neuroimaging-based differential diagnosis
No specific neuroimaging finding has been reported for GBS (Figs. 3, 4, 5), ATM (Figs. 6, 7), and ADEM (Fig. 8) secondary to ZIKV infection. Therefore, it is not possible to recommend ZIKV as the etiology of these neurologic complications just based on the neuroimaging findings; but in combination with the patient history (i.e., active exposure to the virus, and history of symptoms suggestive of ZIKV infection), neuroimaging may be of help to suspect ZIKV infection as the background etiopathogenic agent.
Guillain–Barré syndrome. Spine MRI of a 38-year-old Iranian female with progressive ascending paralysis. Conus medullaris (long arrow), and cauda equina nerve roots (short arrow) appear normal on the sagittal T2-weighted image (a). No signal change is evident on the pre-contrast sagittal T1-weighted image (b), but post-contrast enhancement is noted in the conus medullaris (long arrow), and cauda equina nerve roots (short arrow) following gadolinium-based contrast agent injection (c). Cauda equina nerve roots (arrow) are seen with normal signal on the axial T2-weighted image (d). Conus medullaris, as well as both ventral (solid arrow) and dorsal (dashed arrow) nerve roots show a normal signal on the pre-contrast axial T1-weighted image (e), but post-contrast enhancement is evident in the conus medullaris, as well as ventral (solid arrows) and dorsal (dashed arrows) nerve roots (f). (No definite etiology was suggested for the patient)
Guillain–Barré syndrome. Spine MRI of a 42-year-old Colombian male with asymmetric progressive loss of strength in the right side of his body, and arthralgia. Sagittal (a), and axial (b) contrast-enhanced T1-weighted images show marked enhancement of the cauda equina nerve roots (arrows). (The patient was residing in a ZIKV endemic region, but no confirmatory study was performed. He had history of arthralgia and flu-like symptoms 1 week prior to presentation, which make ZIKV infection the probable etiopathogenic agent)
Guillain–Barré syndrome. Spine MRI of a 64-year-old Colombian female with paresthesia and weakness of the lower limbs, instability in walking, and subsequent difficulty in breathing. There is no obvious signal abnormality on the sagittal T2-weighted (a), and pre-contrast T1-weighted images (b). Enhancement of the cauda equina nerve roots (arrow) is evident following contrast agent injection (c). Compare the pre-contrast (d), and post-contrast (e) axial T1-weighted images for appreciating the cauda equina nerve roots (arrow) enhancement. (The patient was residing in a ZIKV endemic region, but no confirmatory study was performed)
Acute transverse myelitis. Spine MRI of a 22-year-old Iranian male with unsteadiness and lower limbs weakness. A hyperintense ill-defined lesion is seen on the sagittal short-tau inversion recovery image, extending from mid-T9 to mid-T12 (between arrows) and mildly expanding the cord (a). The demyelinating lesion is isointense on the non-contrast enhanced sagittal T1-weighted image (b). On an axial T2-weighted image at the mid-T10 level almost the whole cord (arrow) surface-area is involved and shows a hyperintense signal (c). (No definite etiology was suggested for the patient)
Acute transverse myelitis. Spine MRI of a 60-year-old Colombian female with instability in walking, and a sensory level at the physical examination. A hyperintense expanding lesion (arrow) is seen on the sagittal short-tau inversion recovery (a), and T2-weighted (b) images at the level of T3. The demyelinating lesion (arrow) shows mild enhancement on the contrast-enhanced sagittal T1-weighted image (c). (The patient was residing in a ZIKV endemic region, but no confirmatory study was performed. She had history of shingles, which make varicella zoster the probable etiopathogenic agent)
Acute disseminated encephalomyelitis. Brain MRI of a 14-year-old Colombian boy with acute weakness, paraplegia, bilateral facial paresis, and difficulties in speech. Axial T2-weighted images at different levels (a–c) show multiple hyperintense lesions in bilateral centrum semiovale (arrows in a), periventricular white matter and internal capsule (arrows in b), and pons (arrow in c). The lesions reveal faint post-contrast enhancement (arrow) (d), and show restricted diffusion on the diffusion-weighted image (e) and the apparent diffusion coefficient map (f). (The patient was residing in a ZIKV endemic region, but no confirmatory study was performed. He had history of Dengue vaccination 5 months prior to presentation)
Conclusion
Postnatally acquired ZIKV infection is asymptomatic or mildly symptomatic in most cases, but it may cause life-threatening immune-mediated neurological complications in a few infected patients. So far, no pathognomonic neuroimaging finding has been reported for these conditions in patients with ZIKV infection. Detailed knowledge of the possible neurological complications as well as their neuroimaging manifestations is of paramount importance for an early correct diagnosis and proper management of the affected patients.
References
Zare Mehrjardi M, Poretti A, Keshavarz E. Neuroimaging findings of Zika virus infection: emphasis of congenital versus acquired aspects. Jpn J Radiol. 2017;35(1):41–2.
Zare Mehrjardi M. Neuroimaging findings of Zika virus infection: emphasis of the emerging global threat. Jpn J Radiol. 2017;35(2):87–8.
Zare Mehrjardi M, Poretti A, Huisman TA, Werner H, Keshavarz E, Araujo Júnior E. Neuroimaging findings of congenital Zika virus infection: a pictorial essay. Jpn J Radiol. 2017;35(3):89–94.
Pascuzzi RM, Fleck JD. Acute peripheral neuropathy in adults. Guillain-Barré syndrome and related disorders. Neurol Clin. 1997;15(3):529–47.
Zare Mehrjardi M, Keshavarz E, Poretti A, Hazin AN. Neuroimaging findings of Zika virus infection: a review article. Jpn J Radiol. 2016;34(12):765–70.
Cao-Lormeau VM, Blake A, Mons S, et al. Guillain-Barré syndrome outbreak associated with Zika virus infection in French Polynesia: a case-control study. Lancet. 2016;387(10027):1531–9.
Parra B, Lizarazo J, Jiménez-Arango JA, et al. Guillain-Barré syndrome associated with Zika virus infection in Colombia. N Engl J Med. 2016;375(16):1513–23.
Mahecha MP, Ojeda E, Vega DA, Sarmiento-Monroy JC, Anaya JM. Guillain-Barré syndrome in Colombia: where do we stand now? Immunol Res. 2016. doi:10.1007/s12026-016-8816-8 (Epub ahead of print).
Oehler E, Watrin L, Larre P, Leparc-Goffart I, Lastere S, Valour F. Zika virus infection complicated by Guillain-Barré syndrome case report, French Polynesia, December 2013. Euro Surveill. 2014;19:20720.
Fontes CA, Dos Santos AA, Marchiori E. Magnetic resonance imaging findings in Guillain-Barré syndrome caused by Zika virus infection. Neuroradiology. 2016;58(8):837–8.
Palacios E, Clavijo-Prado C, Ruiz A, Arias Antun A, Julián Duran E. Longitudinal extensive transverse myelitis and Zika virus: a diagnostic challenge in a hospital in Colombia. Neurologia. 2016. doi:10.1016/j.nrl.2016.08.006 (Epub ahead of print).
Mécharles S, Herrmann C, Poullain P, et al. Acute myelitis due to Zika virus infection. Lancet. 2016;387(10026):1481.
Carteaux G, Maquart M, Bedet A, et al. Zika virus associated with meningoencephalitis. N Engl J Med. 2016;374(16):1595–6.
Schwartzmann PV, Ramalho LN, Neder L, et al. Zika virus meningoencephalitis in an immunocompromised patient. Mayo Clin Proc. 2017;92(3):460–6.
Soares CN, Brasil P, Carrera RM, et al. Fatal encephalitis associated with Zika virus infection in an adult. J Clin Virol. 2016;83:63–5.
Kumar S, Misra UK, Kalita J, Salwani V, Gupta RK, Gujral R. MRI in Japanese encephalitis. Neuroradiology. 1997;39(3):180–4.
Petropoulou KA, Gordon SM, Prayson RA, Ruggierri PM. West Nile virus meningoencephalitis: MR imaging findings. AJNR Am J Neuroradiol. 2005;26(8):1986–95.
Niemeyer B, Niemeyer R, Borges R, Marchiori E. Acute disseminated encephalomyelitis following Zika virus infection. Eur Neurol. 2016;77(1–2):45–6.
Acknowledgements
In memory of Dr. Andrea Poretti (April 12, 1977–March 20, 2017), associate professor of radiology and radiological sciences at Johns Hopkins University School of Medicine, and a brilliant physician-scientist in the field of pediatric neurology and neuroimaging.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest.
About this article
Cite this article
Zare Mehrjardi, M., Carteaux, G., Poretti, A. et al. Neuroimaging findings of postnatally acquired Zika virus infection: a pictorial essay. Jpn J Radiol 35, 341–349 (2017). https://doi.org/10.1007/s11604-017-0641-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-017-0641-z