Abstract
Arterial spin labeling (ASL) is a non-contrast method of measuring cerebral perfusion with MRI. It has several advantages over traditional contrast-based perfusion-weighted imaging, including non-invasiveness, more straightforward cerebral blood flow (CBF) quantification, and repeatability. However, because of its lower signal-to-noise ratio (SNR) per unit time and its high sensitivity to arterial transit delays, it has not been used frequently in acute stroke, where arterial delays and time-efficiency are of the essence. This is beginning to change, driven by higher SNR implementations of ASL and the increasing use of 3T scanners. Furthermore, velocity-selective ASL sequences that are largely insensitive to arrival times are beginning to be applied to patients with cerebrovascular disease and promise the ability to quantify CBF even in regions supplied by late-arriving collateral flow. Despite these advances, many practical issues must be addressed to optimize ASL for its use in acute stroke studies. These include optimizing the trade-off between time, SNR, imaging resolution, and sensitivity to slow flow. Rapid and robust post-processing of image data must be made routine, such that CBF maps are available in real time so that they can be considered when making treatment decisions. Lastly, automated software needs to be developed in order to delineate hypoperfused tissue volumes, which is challenging due to the inherent differences between gray and white matter CBF. Attention to these details is critical to translate this promising research tool into mainstream clinical trials and practice in acute stroke.
Similar content being viewed by others
Introduction
Evaluating brain perfusion is an important part of the acute stroke workup with MRI, as prior studies have shown that critically hypoperfused tissue can go onto irreversible infarction in the absence of early reperfusion [1, 2]. The first studies that provided this information were based on the analysis of the MR signal changes caused by an intravenous bolus of a gadolinium-containing contrast agent [3, 4]. This approach has been termed bolus perfusion-weighted imaging (PWI). As these high magnetic susceptibility agents traverse through the brain capillary network, signal loss occurs due to the presence of magnetic field gradients between the vessels and the extravascular space, which is sampled using a fast MRI method using a repetition time on the order of 1–2 s. Since the bolus passes through the brain parenchyma within several seconds, a complete PWI scan rarely lasts over a minute or two. The signal loss induced by the bolus can be related to the tissue concentration which, coupled with a measurement of the arterial delivery of the agent (the arterial input function [AIF]), is used to estimate multiple hemodynamic parameters, including the relative cerebral blood volume, relative cerebral blood flow (CBF), and mean transit time. Additionally, measurements of the delay of the agent arrival can be measured, either directly (the time-to-peak signal or TTP) or via deconvolution with the AIF (Tmax). These latter parameters appear to have good discriminant power between normal tissue and tissue at risk of infarction in the absence of early reperfusion [5, 6]. Based on this, diffusion–perfusion mismatch-based acute stroke trials have been performed using automated software [7]. This approach has become a mainstay of stroke triage with MRI in academic medical centers.
While the principles and first implementation of arterial spin labeling (ASL) to measure perfusion were demonstrated at about the same time as bolus PWI [8, 9], it has yet to be applied to a clinical trial of acute stroke. Why is this? It could be argued that the initial implementations of ASL were particularly ill-suited for stroke studies. They had relatively poor SNR per unit time, partially based on the fact that only 1.5 T scanners were in routine clinical practice at the time. Scan time was upwards of 5 min, which was considered to be too time-consuming for inclusion in an acute stroke MR exam, in which a total of 10 min of imaging time is typical [10]. Additionally, the highest SNR implementation, using a continuous labeling pulse (so-called continuous arterial spin labeling), were very hardware-intensive, as RF amplifiers built to provide pulsed signals could not sustain continuous RF levels without causing damage to either the amplifier or unduly heating the patient. Finally, and perhaps most crucially, ASL was plagued by its high sensitivity to differences in arterial arrival time, since the label decays with the blood T1, which is on the same order or is smaller than the inherent delays between healthy and ischemic tissue in acute stroke. This leads to an underestimation of CBF in regions with long arterial arrival time, potentially overestimating the volume of at-risk tissue.
Why is ASL being revived as a potentially useful tool in the MR workup for acute stroke? One obvious consideration is the recognition that gadolinium-based contrast agents are contraindicated in patients with renal failure due to the risk of nephrogenic systemic fibrosis, first recognized in 2006 [11]. Since renovascular disease and cerebrovascular disease are often comorbid conditions, this limits the number of acute stroke patients that can get a bolus PWI examination. In these patients, ASL is the only perfusion study that is available with MRI. But how about using ASL in those without renal failure? Is there an advantage to doing both ASL and PWI? And what are the problems that have been solved and what practical issues remain? These are the topics that are addressed systematically in this study.
How Long Will It Take?
Time is of the essence in the acute stroke workup. Most published MR-based stroke protocols involve about 8–10 min of imaging time, which translates to about 15–20 min of real time, which includes patient transfer, hookup to power injector for contrast, pre-scan, etc. Results of the examination are usually interpreted in quasi-real time, since the scan is typically a decision point in the patient's triage. At our institution, the most common question is whether the patient would be a good candidate for intra-arterial tissue plasminogen activator (tPA) or mechanical thrombolysis therapy. There is evidence that the MR examination can also select patients who will respond to intravenous (IV) tPA outside of the traditional 3–4.5 h window of time from onset [2, 12, 13].
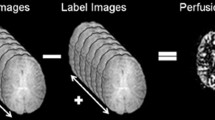
Arterial spin labeling has traditionally required about 5–6 min to acquire a set of whole brain images with sufficient SNR for interpretation. This includes the imaging time required to obtain equilibrium magnetization maps that are required to scale the difference images (control minus label conditions) to create a quantitative CBF map. Our current protocol for 1.5 T imaging, for example, takes 5 min and 55 s. The nominal spatial resolution of these axial images is approximately 3.4 mm in-plane and 6 mm through-plane; approximately 36 slices are acquired in the superior–inferior direction using a 3D stack-of-spiral acquisition and pseudocontinuous labeling [14]. At 3 T, because of the higher inherent SNR, we choose to acquire images with slightly thinner slice thickness (4 mm) and similar in-plane resolution (3 mm), corresponding to an overall imaging time that is somewhat shorter (4 min and 37 s). ASL image quality, as shown in Fig. 1, is markedly improved by moving to higher field strength, due to the higher baseline magnetization available and the longer T1 of the blood, which preserves the magnetization label. The complete details of this ASL implementation are described in Table 1, which includes all of the sequences in our current MR stroke protocol.
An example of ASL images acquired in clinical patients without obvious perfusion pathology at 1.5 T (a) and 3 T (b), using a 3D fast spin-echo background-suppressed pseudocontinuous labeling sequence. Images at 1.5 T required approximately 6 min to acquire, while the 3 T images required about 4.5 min. It should be noted that the improved SNR of the 3 T images is due to both the inherent higher signal sensitivity at and the longer blood T1 at higher field
From this discussion, it is clear that including the ASL sequence would increase the imaging time of the acute stroke MR protocol by about 50 %. It should be noted that this is a smaller percentage of the overall time of the examination, if one includes the time for setup. In fact, if only ASL needs to be performed, there is additional time saving since no IV hookup is required. Also, the ASL sequence parameters listed above are those we employ in all patients, mainly to keep things as simple as possible for our technologists. However, if this imaging time is considered prohibitive, it is possible to reduce the spatial resolution and thereby reduce the imaging time to achieve equivalent SNR. For example, if 8-mm slice thickness is considered reasonable at 3 T, ASL imaging times on the order of 2–3 min become feasible. This flexibility to trade off imaging time against SNR is one of the attractive features of the ASL method in general, a feature not possible with bolus PWI due to the finite, short time duration of the bolus through the capillary bed.
What About Imaging Slow Flow?
The next big practical matter to address is the fact that most implementations of ASL currently available yield erroneous quantitative results in regions where the time for the blood to travel between the site of labeling and the imaged slice is prolonged on the order of the combined labeling time plus post-label delay interval [15, 16]. In our implementation, that time is only about 3.5 s (labeling time 1.5 s + post-label delay 2.0 s). Arterial delays longer than this are common in acute ischemic stroke due to large vessel occlusion and pial collateralization. For example, in many bolus contrast PWI stroke studies, a time-to-peak or Tmax cutoff of 4–6 s appears to provide a good volume estimate of critically hypoperfused tissue. Another problem is that slow flow can be either underestimated (if the delay is very long or if vascular suppression techniques are used) or can appear heterogeneous, with high signal in sluggish feeding arteries and low signal in distal parenchyma if vascular suppression is not used (Fig. 2). This issue will be further discussed in the next section.
Scan on a seventy-three-year-old man with acute stroke caused by occlusion of an M2 branch of the right middle cerebral artery. a DWI shows a small right parietal infarct. b Bolus PWI shows a larger region with perfusion abnormality. c Non-vessel-suppressed and d vessel-suppressed pcASL demonstrate different appearances. The high ASL signal in the periphery of the lesion represents slow flow in collateral vessels. In our experience, this information about collateral networks is useful in the acute stroke setting
To some extent, the CBF underestimation effect in ASL is unimportant if the goal is qualititative assessment of the region of hypoperfused tissue; in fact, it leads to increased contrast between normal and abnormal regions. The problem is that there is probably a range of mildly delayed flow that does not meet the bolus PWI Tmax or TTP criteria for at-risk tissue but still will appear hypoperfused on an ASL study (Fig. 3).
Scan on an eighty-six-year-old man with acute stroke in the right hemisphere. The regions of abnormal DWI (a) and critically hypoperfused tissue based on a bolus PWI (b) Tmax threshold of >6 s are largely matched. However, the ASL CBF images (c) demonstrate a larger hypoperfused region suggesting tissue at risk. The reason for the abnormality is that the mildly Tmax-delayed tissue (in the 4–6-s range) is underestimated on the ASL CBF map. Such a patient might benefit from a conventional ASL scan with longer labeling and post-label delay times, or a transit-time insensitive ASL sequence such as velocity-selective ASL (VSASL)
The significance of this has not been well evaluated in stroke ASL studies, but it is clear that it exists [17–20]. A recent study that directly compared ASL to bolus PWI for the determination of mismatch showed that if no mismatch was seen using ASL, it was exceedingly unlikely that a mismatch would be identified with bolus PWI [21]. However, the problem is that if there was a mismatch based on ASL, there was only about a 50 % chance that the exam would be considered a mismatch using PWI. Thus, if diffusion-weighted imaging (DWI) and PWI lesions are matched, there is a chance that this will appear as a mismatch if ASL is used for perfusion, possibly leading to more aggressive treatment than that which would otherwise be offered.
To Crush or Not to Crush?
It is possible to insert crusher gradients or prepare the magnetization such that the ASL signal from moving spins with blood vessels will be suppressed or “crushed” [22–24]. The advantage of this is that the ASL signal that is observed is only due to spins that have been extracted out of the vessels and into the extravascular space of the brain. The degree of suppression can be controlled based on the size and timing of the gradients, with a typical cutoff velocity usually chosen on the order of 4–10 cm/s. The exact velocity cutoff is limited by the fact that as one goes to lower cutoffs, diffusion effects become prominent, leading to a decrease in overall ASL signal-to-noise. It is important to realize that ASL sequences that use a spin-echo readout are inherently vascular-suppressed to some extent, since fast-flowing vessels will not experience both the slice-selective 90° and 180° pulses. Finally, it should be recognized that there is no consensus as to what the correct vascular cutoff value should be, and it is likely that very slow flow through extensive collaterals will be very difficult to suppress using this method. The only solution in these cases is to use an extremely long post-label delay time or a method such as velocity-selective ASL (VSASL). Both of these approaches will be discussed in the next section.
While this effect for the most part will lead to CBF underestimation, if the label is in the feeding arteries at the time of imaging, one can see serpiginous high ASL signal surrounding a darker core lesion (where the labeled spins will ultimately perfuse). This has been termed arterial transit artifact (ATA) [25]. Its localization to the vascular watershed regions, particularly in a bilateral manner, has been dubbed the borderzone ASL sign and is often identified in older patients with reduced cardiac output by using standard labeling and post-labeling delay (PLD) times [26]. ATA is particularly evident in implementations of ASL that do not include vascular crusher gradients to suppress signal in blood flowing above a certain velocity (i.e., non-vessel-suppressed ASL). Currently, the GE 3D pseudocontinuous ASL product implementation does not routinely vessel-suppress; other vendors such as Siemens and Philips have available 2D pulsed ASL scanners that typically employ some degree of vascular crushing.
There are advantages and disadvantages to each approach. Vessel-suppressed ASL avoids the possible confusion that might arise between distinguishing ATA (indicative at some level of compromised perfusion) from luxury perfusion, which also shows high ASL signal; however, these two different patterns are usually easily recognized even on non-vessel-suppressed ASL due to the more uniform appearance of hyperperfusion (Fig. 4). The advantages of non-vessel-suppressed ASL are the generally higher SNR, the ability to detect ATA that yields information on collateral flow, and the ability to use a single methodology to evaluate potential shunt lesions, such as small vascular malformations [27, 28]. One study using non-vessel-suppressed ASL evaluated the qualitative size of the perfusion deficit either including or neglecting ATA, thus trying to mimic the two choices [21]. It was found that for the purposes of comparing with bolus PWI, the simulated vessel-suppressed ASL more closely approximated the PWI mismatch conclusions. With experience, it is usually possible to distinguish slow flow from collaterals from high flow due to reperfusion, and we prefer to use a non-vessel-suppressed ASL sequence. In general, however, one does not usually get to choose this option if you are using a product ASL sequence, since you are dependent upon the vendor.
Example of the different characters of high signal provided from an ASL sequence without vascular suppression in the setting of delayed or collateral flow (a) and hyperperfusion (b). Collateral flow tends to surround a low ASL signal region, and the high signal has a serpiginous appearance outlining the collateral vessels themselves. Hyperperfusion appears more homogeneous and does not surround a low ASL region
What if I Want Quantitative CBF?
In the clinical arena, the importance of the fact that ASL can obtain quantitative CBF remains unclear. While there are exceptions to this (global hyperperfusion states like hypercapnia and post-anoxic brain injury, for example [29]), most of the time, a relative measure gives most of the required information. However, what is critical is that the relative CBF values are accurate, and this is the biggest problem with standard ASL implementations in stroke, since the underestimation and ATA associated with long delays can lead to erroneous conclusions about whether flow levels are too low to maintain cerebral viability. There are two solutions to this, both of which are costly in terms of SNR and/or imaging time.
The first is simple: take your standard ASL and maximize the labeling time and the post-label delay. This will make the images less sensitive to arrival time. An example of this is shown in Fig. 5 for a patient with unilateral Moyamoya disease. Using this product 3D pseudocontinuous ASL sequence, the labeling time cannot be increased (it is set at 1,500 ms). However, while we typically use a PLD of 2,000 ms, this can be increased, and the use of a PLD time of 3,000 ms demonstrates that CBF in the affected region of this patient is actually nearly normal. In our experience, very few patients with normal but delayed flow still show erroneous CBF measurements with this long PLD. However, the price of this insensitivity is high; because the ASL label is experiencing T1 decay, the percent signal change in the ASL difference images decreases, and more averages are required to achieve the same SNR. For example, our 4 min and 37 s standard 2,000 ms PLD ASL imaging time at 3T increases to 8 min and 37 s for the 3,000 ms PLD setting. This makes it suboptimal, due to increased patient motion, and results in the ASL sequence occupying a large time fraction of a rapid acute stroke MR imaging protocol. However, it is a solution, and particularly if time is not of the essence (perhaps in the setting of assessing reperfusion), it is probably the easiest fix.
ASL images in a patient with unilateral Moyamoya disease affecting the left middle cerebral artery territory but with only minimally decreased absolute CBF (based on gold-standard xenon CT examination (not shown). a Conventionally tagged pseudocontinuous ASL (pcASL) with a post-label delay time of 1,500 ms demonstrates a region of apparent hypoperfusion. b The same imaging sequence demonstrates symmetric flow if the post-label delay time is extended to 3,000 ms; however, the imaging time to acquire reasonable SNR is now approximately 9 min. c Velocity-selective ASL (VSASL) using a TI of 1,600 ms shows similar findings to the very long PLD conventionally tagged pcASL image while maintaining the same imaging time (5 min). This suggests that VSASL may have a role in acute stroke ASL imaging
The other approach to minimize transit delay errors is the use of a new class of ASL sequence that labels based on spin velocity rather than spin location [30, 31]. Velocity-selective ASL uses a global velocity-selective labeling pulse to saturate spins moving above a certain velocity cutoff (V cut), which is usually set at about 2 cm/s. Note that the spins are labeled everywhere in the brain rather than in the neck, thus minimizing the effects of transit time. Following a time delay TI (analogous to the PLD in conventional ASL sequences), which allows arterial blood to decelerate and venous blood to accelerate, images of only slow-flowing spins (again based on the parameter V cut) are imaged. Images taken with and without the velocity-selective pulse are subtracted, just like in conventional ASL, in order to provide a CBF measurement. A recent paper demonstrated superior performance of VSASL to depict regions with long arterial delay times in patients with steno-occlusive cerebrovascular disease [32].
While being more insensitive to arrival time, VSASL has some problems that limit general applicability. First, there is no product version of VSASL available from any of the major commercial manufacturers. Second, since the velocity-selective pulse saturates rather than inverts flowing spins, the ultimate achievable SNR is reduced [32]; of course, this is mitigated by the fact that spins do not have to travel very far to the capillary bed, and for this reason, TI can be kept short (our standard stroke protocol uses a TI of 1,600 ms), which buys back some of the SNR loss. In our experience, clinically robust and interpretable CBF images can be acquired with VSASL at 3T in about 5 min (Fig. 5). It should be noted that slow flow effects are probably only mitigated in this approach rather than entirely suppressed, though one has some control over this by varying the sequence parameters [33]. It is possible that VSASL may turn out to be the best ASL approach for acute stroke patients, given the trade-offs between imaging time and CBF quantification.
How Long Will It Take to Get My Results?
For any perfusion study to be useful in stroke, the results need to be available in near real time. The importance of this has been shown for PWI results and will become important for ASL as it is introduced into clinical trials and routine practice [7]. The time constraint in our experience is that the perfusion results should be available within 5 min of the end of the scan. Unlike bolus PWI, which needs to be the last or near last sequence in an acute stroke protocol, ASL can be acquired earlier since it does not require contrast. In fact, probably the best place for ASL is immediately following the DWI or following both the DWI and MRA sequences. This allows more time for post-processing, which can run while the remaining sequences are acquired.
Some vendor implementations come with automated real-time reconstruction, but others require access to a dedicated workstation. Research-based pulse sequences generally require some sort of dedicated “pipeline” in which raw images can be transmitted to an off-line reconstruction, and CBF maps can be returned to the scanner or PACS system [34]. For non-background-suppressed ASL methods, motion correction or removal of motion-contaminated image pairs is essential to avoid swamping the tiny 1 % ASL signal. Finally, automated software that assesses CBF or arrival time measures to produce estimates of viable, at-risk, and infarcted tissue will make these methods more attractive to clinicians who do not have experience with perfusion imaging. Such lesion thresholding methods are challenging for CBF, which varies approximately twofold between normal gray and white matter. Nevertheless, there is experience on creating these maps from the CT perfusion literature that may be applicable to ASL. This is important because objective and quantitative lesion volume measurements are essential for wide-scale implementation of any perfusion imaging method.
ASL—Too Many Flavors?
One of the great strengths of the ASL technique is the incredible flexibility regarding exactly how to implement the labeling process and the readout strategy. However, it can also be a drawback. Clinical studies over the years have been performed with a wide range of ASL methodologies, which yield slightly different CBF values and have different sensitivities and artifacts. This is probably why bolus PWI, which can be much more easily standardized, has been a preferred method in acute stroke trials, especially multicenter trials. If ASL is to have the same impact as PWI in stroke triage, more standardization between vendors and research teams will have to occur. Table 2 outlines the clinical product ASL sequences currently provided by the major manufacturers at the time of writing.
While there are continued debates on many of these issues, the field seems to be coalescing around several ASL approaches. In particular, the improved SNR and reduced hardware demands of pseudocontinuous labeling appear to make it the labeling method of choice for clinical applications. Of course, pseudocontinuous ASL has its own problems, which include reduced labeling efficiency relative to pulsed methods and rare instances of focal poor labeling efficiency of specific arteries; however, the benefits accrued by its higher SNR are substantial and will likely drive its clinical application. Longer PLD sequences are also increasing in popularity (thanks to a desire to minimize arterial arrival time issues), and the growing use of 3T has aided this process.
Despite this, the current situation is that multicenter and multivendor trials using ASL are very challenging, and more studies comparing the results from the more common product implementations, preferably in the same subjects, should be a priority. More communication between researchers using different platforms, perhaps under currently existing organizations such as the Stroke Imaging Repository (stir.ninds.nih.gov) or the ASL network (asl-network.org) would be beneficial. Otherwise, ASL will be limited to small single center studies, and the results will not be transferable to general practice.
Conclusions
This article has summarized the author's experience using ASL in the acute stroke setting. The presence of long arterial arrival times requires attention to specific details of the ASL implementation, especially the optimization of the PLD time. With some experience and knowledge of the expected artifacts, it is possible to accurately interpret ASL findings in these patients. Much of this has been gained by acquiring contemporaneous bolus contrast perfusion imaging, which we recommend in the short term until one becomes comfortable with ASL interpretation. In the longer term, more standardization, particularly between vendors, will be required to realize the full potential of this non-contrast perfusion method in acute stroke.
References
Kidwell CS, Alger JR, Saver JL. Beyond mismatch: evolving paradigms in imaging the ischemic penumbra with multimodal magnetic resonance imaging. Stroke. 2003;34:2729–35.
Albers GW, Thijs VN, Wechsler L, et al. Magnetic resonance imaging profiles predict clinical response to early reperfusion: the diffusion and perfusion imaging evaluation for understanding stroke evolution (DEFUSE) study. Ann Neurol. 2006;60:508–17.
Villringer A, Rosen BR, Belliveau JW, et al. Dynamic imaging with lanthanide chelates in normal brain: contrast due to magnetic susceptibility effects. Magn Reson Med. 1988;6:164–74.
Sorensen AG, Buonanno FS, Gonzalez RG, et al. Hyperacute stroke: evaluation with combined multisection diffusion-weighted and hemodynamically weighted echo-planar MR imaging. Radiology. 1996;199:391–401.
Olivot JM, Mlynash M, Thijs VN, et al. Optimal Tmax threshold for predicting penumbral tissue in acute stroke. Stroke. 2009;40:469–75.
Christensen S, Mouridsen K, Wu O, et al. Comparison of 10 perfusion MRI parameters in 97 sub-6-hour stroke patients using voxel-based receiver operating characteristics analysis. Stroke. 2009;40:2055–61.
Straka M, Albers GW, Bammer R. Real-time diffusion-perfusion mismatch analysis in acute stroke. J Magn Reson Imaging. 2010;32:1024–37.
Detre JA, Leigh JS, Williams DS, Koretsky AP. Perfusion imaging. Magn Reson Med. 1992;23:37–45.
Roberts DA, Detre JA, Bolinger L, Insko EK, Leigh JS. Quantitative magnetic resonance imaging of human brain perfusion at 1.5 T using steady-state inversion of arterial water. Proc Natl Acad Sci. 1994;91:33–7.
Hjort N, Butcher K, Davis SM, et al. Magnetic resonance imaging criteria for thrombolysis in acute cerebral infarct. Stroke. 2005;36:388–97.
Bongartz G. Imaging in the time of NFD/NSF: do we have to change our routines concerning renal insufficiency? Magma. 2007;20:57–62.
Davis SM, Donnan GA, Parsons MW, et al. Effects of alteplase beyond 3 h after stroke in the Echoplanar Imaging Thrombolytic Evaluation Trial (EPITHET): a placebo-controlled randomised trial. Lancet Neurol. 2008;7:299–309.
Schellinger PD, Fiebach JB, Hacke W. Imaging-based decision making in thrombolytic therapy for ischemic stroke: present status. Stroke. 2003;34:575–83.
Dai W, Garcia D, de Bazelaire C, Alsop DC. Continuous flow driven inversion for arterial spin labeling using pulsed radiofrequency and gradient fields. Magn Reson Med. 2008;60:1488–97.
Hendrikse J, van Osch MJ, Rutgers DR, et al. Internal carotid artery occlusion assessed at pulsed arterial spin-labeling perfusion MR imaging at multiple delay times. Radiology. 2004;233:899–904.
Bokkers RP, van der Worp HB, Mali WP, Hendrikse J. Noninvasive MR imaging of cerebral perfusion in patients with a carotid artery stenosis. Neurology. 2009;73:869–75.
Siewert B, Schlaug G, Edelman RR, Warach S. Comparison of EPISTAR and T2*-weighted gadolinium-enhanced perfusion imaging in patients with acute cerebral ischemia. Neurology. 1997;48:673–9.
Chalela JA, Alsop DC, Gonzalez-Atavales JB, Maldjian JA, Kasner SE, Detre JA. Magnetic resonance perfusion imaging in acute ischemic stroke using continuous arterial spin labeling. Stroke. 2000;31:680–7.
Wang DJ, Alger JR, Qiao JX, et al. The value of arterial spin-labeled perfusion imaging in acute ischemic stroke—comparison with dynamic susceptibility contrast-enhanced MRI. Stroke. 2012;43:1018–24.
Deibler AR, Pollock JM, Kraft RA, Tan H, Burdette JH, Maldjian JA. Arterial spin-labeling in routine clinical practice, part 2: hypoperfusion patterns. AJNR Am J Neuroradiol. 2008;29:1235–41.
Zaharchuk G, El Mogy I, Fischbein N, Albers G. Comparison of arterial spin labeling and bolus perfusion-weighted imaging for detecting mismatch in acute stroke. Stroke. 2012; in press
Wang J, Alsop DC, Song HK, et al. Arterial transit time imaging with flow encoding arterial spin tagging (FEAST). Magn Reson Med. 2003;50:599–607.
Petersen ET, Lim T, Golay X. Model-free arterial spin labeling quantification approach for perfusion MRI. Magn Reson Med. 2006;55:219–32.
Zaharchuk G, Shankaranarayanan A, Alsop DC. Removing large vessel contamination from arterial spin label MR perfusion images using T2 preparation. In Proc Radiological Society of. North America. Chicago, IL. 2008:VN31-10
Detre JA, Samuels OB, Alsop DC, Gonzalez-At JB, Kasner SE, Raps EC. Noninvasive magnetic resonance imaging evaluation of cerebral blood flow with acetazolamide challenge in patients with cerebrovascular stenosis. J Magn Reson Imaging. 1999;10:870–5.
Zaharchuk G, Bammer R, Straka M, et al. Arterial spin-label imaging in patients with normal bolus perfusion-weighted MR imaging findings: pilot identification of the borderzone sign. Radiology. 2009;252:797–807.
Wolf RL, Wang J, Detre JA, Zager EL, Hurst RW. Arteriovenous shunt visualization in arteriovenous malformations with arterial spin-labeling MR imaging. AJNR Am J Neuroradiol. 2008;29:681–7.
Le TT, Fischbein NJ, Andre JB, Wijman C, Rosenberg J, Zaharchuk G. Identification of venous signal on arterial spin labeling improves diagnosis of dural arteriovenous fistulas and small arteriovenous malformations. AJNR Am J Neuroradiol. 2012;33:61–8.
Deibler AR, Pollock JM, Kraft RA, Tan H, Burdette JH, Maldjian JA. Arterial spin-labeling in routine clinical practice, part 3: hyperperfusion patterns. AJNR Am J Neuroradiol. 2008;29:1428–35.
Wong EC, Cronin M, Wu W-C, Inglis B, Frank LR, Liu TT. Velocity-selective arterial spin labeling. Magn Reson Med. 2006;55:1334–41.
Duhamel G, de Bazelaire C, Alsop DC. Evaluation of systematic quantification errors in velocity-selective arterial spin labeling of the brain. Magn Reson Med. 2003;50:145–53.
Qiu D, Straka M, Zun Z, Bammer R, Moseley ME, Zaharchuk G. CBF measurements using multidelay pseudocontinuous and velocity-selective arterial spin labeling in patients with long arterial transit delays: comparison with xenon CT CBF. J Magn Reson Imaging. 2012. doi:10.1002/jmri.23613.
Wu WC, Wong EC. Intravascular effect in velocity-selective arterial spin labeling: the choice of inflow time and cutoff velocity. NeuroImage. 2006;32:122–8.
Deibler AR, Pollock JM, Kraft RA, Tan H, Burdette JH, Maldjian JA. Arterial spin-labeling in routine clinical practice, part 1: technique and artifacts. AJNR Am J Neuroradiol. 2008;29:1228–34.
Luh WM, Wong EC, Bandettini PA, Hyde JS. QUIPSS II with thin-slice TI1 periodic saturation: a method for improving accuracy of quantitative perfusion imaging using pulsed arterial spin labeling. Magn Reson Med. 1999;41:1246–54.
Acknowledgments
This work was supported by multiple NIH grants (R01-NS066506, R01-NS047607), by GE Healthcare, and the Lucas foundation.
Conflict of Interest
The author is a member of the Neuroradiology Advisory Board for GE Healthcare and also receives research support from GE Healthcare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zaharchuk, G. Arterial Spin Labeling for Acute Stroke: Practical Considerations. Transl. Stroke Res. 3, 228–235 (2012). https://doi.org/10.1007/s12975-012-0159-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-012-0159-8