Abstract
Objective:
A substantial number of children exposed to gestational opioids have neurodevelopmental, behavioral and cognitive problems. Opioids are not neuroteratogens but whether they affect the developing brain in more subtle ways (for example, volume loss) is unclear. We aimed to determine the feasibility of using magnetic resonance imaging (MRI) to assess volumetric changes in healthy opioid-exposed infants.
Study design:
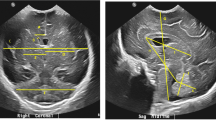
Observational pilot cohort study conducted in two maternity hospitals in New South Wales, Australia. Maternal history and neonatal urine and meconium screens were obtained to confirm drug exposure. Volumetric analysis of MRI scans was performed with the ITK-snap program.
Result:
Scans for 16 infants (mean (s.d.) gestational age: 40.9 (1.5) weeks, birth weight: 3022.5 (476.6) g, head circumference (HC): 33.7 (1.5 cm)) were analyzed. Six (37.5%) infants had HC <25th percentile. Fourteen mothers used methadone, four used buprenorphine and 11 used more than one opioid (including heroin, seven). All scans were structurally normal whole brain volumes (357.4 (63.8)) and basal ganglia (14.5 (3.5)) ml were significantly smaller than population means (425.4 (4.8), 17.1 (4.4) ml, respectively) but lateral ventricular volumes (3.5 (1.8) ml) were larger than population values (2.1(1.5)) ml.
Conclusion:
Our pilot study suggests that brain volumes of opioid-exposed babies may be smaller than population means and that specific regions, for example, basal ganglia, that are involved in neurotransmission, may be particularly affected. Larger studies including correlation with neurodevelopmental outcomes are warranted to substantiate this finding.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
United Nations. Office on Drugs and Crime (UNODC) World Drug Report 2013. Available from www.unodc.org (Accessed 10 October 2013).
O'Donnell M, Nassar N, Leonard H, Hagan R, Mathews R, Patterson Y et al. Increasing prevalence of neonatal withdrawal syndrome: population study of maternal factors and child protection involvement. Pediatrics 2009; 123: e614–e621.
Finnegan LP, Connaughton JF Jr, Kron RE . Neonatal abstinence syndrome: assessment and management. Addict Dis 1975; 2: 141–158.
Patrick SW, Schumacher RE, Benneyworth BD, Krans EE, McAllister JM, Davis MM et al. Neonatal Abstinence Syndrome and Associated Health Care Expenditures United States, 2000-2009. JAMA 2012; 307: 1934–1940.
Ornoy A, Tahover E, Finkel-Pekarsky V, Arnon J, Kennedy D, Erebara A, Einarson A et al. The developmental outcome of children born to heroin-dependent mothers, raised at home or adopted. Child Abuse Negl 1996; 20: 385–396.
Rounsaville BJ, Kosten TR, Weissman MM, Prusoff B, Pauls D, Anton SF et al. Psychiatric disorders in relatives of probands with opiate addiction. Arch Gen Psychiatry 1991; 48: 33–42.
Hu S, Sheng WS, Lokensgard JR, Peterson PK . Morphine induces apoptosis of human microglia and neurons. Neuropharmacology 2002; 42: 829–836.
Bora E, Yücel M, Fornito A, Pantelis C, Harrison BJ, Cocchi L et al. White matter microstructure in opiate addiction. Addict Biol 2012; 17 (1): 141–148.
Lu R, Liu X, Long H, Ma L . Effects of prenatal cocaine and heroin exposure on neuronal dendrite morphogenesis and spatial recognition memory in mice. Neurosci Lett 2012; 522: 128–133.
Xu B1, Wang Z, Li G, Li B, Lin H, Zheng R et al. Heroin-administered mice involved in oxidative stress and exogenous antioxidant-alleviated withdrawal syndrome. Basic Clin Pharmacol Toxicol 2006; 99 (2): 153–161.
Qiu Y, Jiang G, Su H, Lv X, Zhang X, Tian J et al. Progressive white matter microstructure damage in male chronic heroin dependent individuals: a DTI and TBSS study. Plos One 2013; 8: e63212.
McGlone L, Hamilton R, McCulloch DL, Boulton R, Bradnam MS, Weaver LT et al. Neonatal visual evoked potentials in infants born to mothers prescribed methadone. Pediatrics 2013; 131 (3): e857–6.
Pasto ME, Graziani LJ, Tunis SL, Deiling JM, Kurtz AB, Goldberg B et al. Ventricular configuration and cerebral growth in infants born to drug-dependent mothers. Pediatr Radiol 1985; 15: 77–81.
Kahila H, Kivitie-Kallio S, Halmesmäki E, Valanne L, Autti T . Brain magnetic resonance imaging of infants exposed prenatally to buprenorphine. Acta Radiol 2007; 48: 228–231.
Walhovd KB, Watts R, Amlien I, Woodward LJ . Neural tract development of infants born to methadone-maintained mothers. Pediatr Neurol 2012; 47: 1–6.
Walhovd KB, Moe V, Slinning K, Due-Tønnessen P, Bjørnerud A, Dale AM et al. Volumetric cerebral characteristics of children exposed to opiates and other substances in utero. Neuroimage 2007; 36 (4): 1331–1344.
Golan A, Marco R, Raz H, Shany E . Imaging in the newborn: infant immobilizer obviates the need for anesthesia. Isr Med Assoc J 2011; 13: 663–665.
Yushkevich PA, Piven J, Hazlett HC, Smith RG, Ho S, Gee JC et al. User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. Neuroimage 2006; 31: 1116–1128.
Knickmeyer RC, Gouttard S, Kang C, Evans D, Wilber K, Smith JK et al. A structural MRI study of human brain development from birth to 2 years. J Neurosci 2008; 28: 12176–12182.
Zacharia A, Zimine S, Lovblad KO, Warfield S, Thoeny H, Ozdoba C et al. Early assessment of brain maturation by MR imaging segmentation in neonates and premature infants. AJNR Am J Neuroradiol 2006; 27: 972–977.
Konijnenberg C, Melinder A . Prenatal exposure to methadone and buprenorphine: a review of the potential effects on cognitive development. Child Neuropsychol 2011; 17: 495–519.
Zagon IS, Verderame MF, McLaughlin PJ . The biology of the opioid growth factor receptor (OGFr). Brain Res Rev 2002; 38: 351–376.
Golalipour MJ, Ghafari S . Purkinje cells loss in off spring due to maternal morphine sulfate exposure: a morphometric study. Anat Cell Biol 2012; 45: 121–127.
Upadhyay J, Maleki N, Potter J, Elman I, Rudrauf D, Knudsen J et al. Alterations in brain structure and functional connectivity in prescription opioid-dependent patients. Brain 2010; 133: 2098–2114.
Lin WC, Chou KH, Chen HL, Huang CC, Lu CH, Li SH et al. Structural deficits in the emotion circuit and cerebellum are associated with depression, anxiety and cognitive dysfunction in methadone maintenance patients: a voxel-based morphometric study. Psychiatry Res 2012; 201: 89–97.
Dong Z1, Cao J, Xu L . Opiate withdrawal modifies synaptic plasticity in subicular-nucleus accumbens pathway in vivo. Neuroscience 2007; 144 (3): 845–854.
Bartlett E . Chasing ‘chasing the dragon’ with MRI: leukoencephalopathy in drug abuse. Br J Radiology 2005; 78: 997–1004.
Younger JW, Chu LF, D'Arcy NT, Trott KE, Jastrzab LE, Mackey SC et al. Prescription opioid analgesics rapidly change the human brain. Pain 2011; 152 (8): 1803–1810.
Mills F, MacLennan SC, Devile CJ, Saunders DE . Severe cerebellitis following methadone poisoning. Pediatr Radiol 2008; 38: 227–229.
Lind A, Parkkola R, Lehtonen L, Munck P, Maunu J, Lapinleimu H et al. Associations between regional brain volumes at term-equivalent age and development at 2 years of age in preterm children. Pediatr Radiol 2011; 41 (8): 953–956.
Räikkönen K, Forsén T, Henriksson M, Kajantie E, Heinonen K, Pesonen AK et al. Growth trajectories and intellectual abilities in young adulthood: The Helsinki Birth Cohort study. Am J Epidemiol 2009; 170 (4): 447–455.
Acknowledgements
We thank Ms Eszter Jozsa and Ms Joanna Michalowski for helping us conduct the MRI scans. This study was funded by the Cornucopia Foundation of the Royal Hospital for Women and the Langton Centre, South East Sydney Local Health District, New South Wales, Australia.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
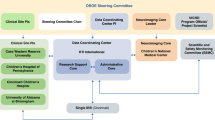
BOB COLLABORATIVE GROUP M Pham, S Lees, R Nanan, B Fonseca, A Lovett, M Abdel-Latif, J Sinn, C Maher, J Stack, K Yates, S Clews, J Falconer, C Rae, J Fullerton, P Schofield, I Wright, K Kaltenbach, J Feller, J Lee Oei
Rights and permissions
About this article
Cite this article
Yuan, Q., Rubic, M., Seah, J. et al. Do maternal opioids reduce neonatal regional brain volumes? A pilot study. J Perinatol 34, 909–913 (2014). https://doi.org/10.1038/jp.2014.111
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2014.111
This article is cited by
-
Ultrasound evaluation of brain parenchyma in preterm infants with prenatal opioid exposure
Journal of Perinatology (2023)
-
Outcomes of Babies with Opioid Exposure (OBOE): protocol of a prospective longitudinal cohort study
Pediatric Research (2023)
-
Intrauterine Drug Exposure—What the Pediatrician Needs to Know
Current Treatment Options in Pediatrics (2023)
-
Neonatal opioid toxicity: opioid withdrawal (abstinence) syndrome with emphasis on pharmacogenomics and respiratory depression
Archives of Toxicology (2023)
-
Alterations of brain microstructures in a mouse model of prenatal opioid exposure detected by diffusion MRI
Scientific Reports (2022)