Abstract
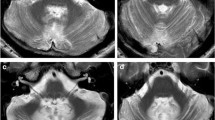
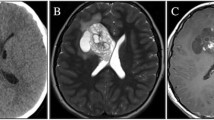
The posterior fossa syndrome (PFS) consists of a variety of symptoms, including cerebellar mutism, behavioral disturbances and personality changes. We report longitudinal clinical, neuroradiological and neurobehavioral findings in a 19-year-old left-handed patient, diagnosed with attentional deficit hyperactivity disorder (ADHD) at the age of 12, who underwent posterior fossa tumor resection. Although the patient did not develop cerebellar mutism after surgery, marked apathy and emotional indifference, urinary retention, eye-lid apraxia and visual hallucinosis became apparent after a brief interval of normal functioning. Based on these findings it is argued that the PFS might be considered a semiological heterogeneous condition with variable clinical expressions. Long-term follow-up investigations revealed subtle, but significant cognitive and affective deficits, resembling the cerebellar cognitive affective syndrome in adults. As demonstrated by functional neuroimaging studies with SPECT, symptoms were associated with perfusional deficits in the anatomoclinically suspected supratentorial regions, reflecting the distant impact of the cerebellum on cognitive and affective functions.
Similar content being viewed by others
References
Daly DD, Love JG. Akinetic mutism. Neurology. 1958;8: 238–42.
Rekate HL, Grubb RL, Aram DM. Muteness of cerebellar origine. Arch Neurol. 1985;42:697–8.
Ersahin Y, Mutluer S, Saydam S, Barcin E. Cerebellar mutism: Report of two unusual cases and review of the literature. Clin Neurol Neurosurg. 1996;99:130–4.
Al-Anazi A, Hassounah M, Sheikh B, Barayan S. Cerebellar mutism caused by arteriovenous malformation of the vermis. Br J Neurosurg. 2001;15:47–50.
Riva D. The cerebellar contribution to language and sequential functions: Evidence from a child with cerebellitis. Cortex. 1998;34:279–87.
Pollack IF. Posterior fossa syndrome. Int Rev Neurobiol. 1997;41:411–32.
Catsman-Berrevoets C, Van DongenHR, Mulder PGH, Pas y Geuze D, Paquier PF, Lequin MH. Tumor type and size are high risk factors for the syndrome of cerebellar mutism and subsequent dysarthria. J Neurol Neurosurg Psych. 1999;67:755–7.
Pollack IF, Polinko P, Albright AL, Towbin R, Fitz C. Mutism and pseudobulbar symptoms after resection of posterior fossa tumors in children: Incidence and pathophysiology. Neurosurgery. 1995;37:885–93.
Riva D, Giorgi C. The cerebellum contributes to higher functions during development. Evidence from a series of children surgically treated for posterior fossa tumours. Brain. 2000;123:1051–61.
Ozimek A, Richter S, Hein-Kropp C, Schoch B, Goriben B, Kaiser O, et al. Cerebellar mutism. Report of four cases. J Neurol. 2004;251:963–72.
Wechsler D. Wechsler Adult Intelligence Scale — Revised (WAIS-R). San Antonio: The Psychological Corporation, 1981.
Wechsler D, Stone CP. Wechsler Memory Scale — Revised (WMS-R). San Antonio: The Psychological Corporation, 1987.
Heaton RK, Chelune GJ, Talley JL, Kay GG, Curtiss G. Wisconsin Card Sorting Test: Revised and expanded. Lutz: Psychological Assessment Resources Inc, 1993.
Hammes JGW. Stroop Kleur Woord Test. Lisse: Swets Zeitlinger BV, 1971.
Reitan RM. Validity of the Trail Making Test as an indicator of organic brain damage. Percep Motor Skills. 1958;8:271–6.
Brickenkamp R, Zilmer E. d2 — Test of Attention Hogrefe & Huber Publishers, Göttingen, 1998.
Osterrieth PA. Rey’s Complexe Figuur Test. Amsterdam: Swets Zeitlinger Publishers, 1994.
Kaplan E, Goodglass H, Weintraub S. Boston Naming Test. USA: Lea and Febiger, 1983.
Mariën P, Mampaey E, Vervaet A, Saerens J, De Deyn PP. Normative data for the Boston Naming Test in Native Dutch speaking Belgian elderly. Brain Lang. 1998;65: 447–67.
Berquin PC, Giedd JN, Jacobsen LK, Hamburger SD, Krain AL, Rapoport JL, et al. Cerebellum in attention-deficit hyperactivity disorder: a morphometric MRI study. Neurology. 1998;50:1087–93.
Kim BN, Lee JS, Shin MS, Cho SC, Lee DS. Regional cerebral perfusion abnormalities in attention deficit/hyperactivity disorder. Statistical parametric mapping analysis. Eur Arch Psych Clin Neurosci. 2002;252:219–25.
Turkel SB, Chen LS, Nelson MD, Hyder D, Gilles FH, Woodall L, et al. Case series: Acute mood symptoms associated with posterior fossa lesions in children. J Neuropsych Clin Neurosci. 2004;16:443–5.
Levinsohn L, Cronin-Golomb A, Schmahmann JD. Neuropsychological consequences of cerebellar tumor resection in children: Cerebellar cognitive affective syndrome in a paediatric population. Brain. 2000;123:1041–50.
Sadeh M, Cohen I. Transient loss of speech after removal of posterior fossa tumors: One aspect of a larger neuropsychological entity: the cerebellar cognitive affective syndrome. Pediatr Hemat Oncol. 2000;18:423–6.
Sinha AK, Rajender Y, Dinaker I. Transient cerebellar mutism after evacuation of a spontaneous vermian haematoma. Child Nerv Syst. 1998;14:460–2.
Siffert J, Poussaint TY, Goumnerova LC, Scott RM, LaValley B, Tarbell NJ, et al. Neurological dysfunction associated with postoperative cerebellar mutism. J Neuro-Oncol. 2000;48:75–81.
Humphreys RP. Mutism after posterior fossa surgery. In: Marlin AE, editor. Concepts in pediatric neurosurgery. Karger: Basel, 1989, vol 9, pp 57–64.
Gaskill SJ, Marlin AE. Transient eye closure after posterior fossa tumor surgery in children. Pediatr Neurosurg. 1991— 92;17:196–8.
Pollack IF. Neurobehavioral abnormalities after posterior fossa surgery in children. Int Rev Psych. 2001;13:302–12.
Catsman-Berrevoets CE, Van Dongen HR, Aarsen FK, Paquier PF. Transient cerebellar eye closure and mutism after cerebellar tumor surgery: Long-term clinical follow-up of neurologic and behavioral disturbances in a 14-year-old girl. Pediatr Neurosurg. 2003;38:122–7.
Daniels SR, Moores LE, DiFazio MP. Visual disturbance associated with postoperative cerebellar mutism. Pediatr Neurol. 2005;32:127–30.
Kirk EA, Howard VC, Scott CA. Description of posterior fossa syndrome in children after posterior fossa brain tumor surgery. J Pediatr Oncol Nurs. 1995;12:181–7.
Gangemi M, Maiuri F, Sigona L, Sardo L. Mutism after surgery for posterior fossa tumors in children. Neurol Psych Brain Res. 2000;8:37–42.
Holman E. Difficult urination associated with intracranial tumors of the posterior fossa. Arch Neurol Psych. 1926;15: 371–80.
Ronning C, Sundet K, Due-Tonnessen B, Lundar T, Helseth E. Persistent cognitive dysfunction secondary to cerebellar injury in patients treated for posterior fossa tumors in childhood. Pediatr Neurosurg. 2005;41:15–21.
Schmahmann JD, Sherman JC. The cerebellar cognitive affective syndrome. Brain. 1998;121:561–79.
Algoed L, Janssens J. Vanhooren G. Apraxia of eye lid opening secondary to right frontal infarction. Acta Neurol Belgica. 1992;92:228–33.
Rinaldi I, Botton JE, Troland CE. Cortical visual disturbances following ventriculography and/or ventricular decompression. J Neurosurg. 1962;19:568–76.
Liu GT, Phillips PC, Molloy PT, Needle MN, Galetta SL, Balcer LJ, et al. Visual impairment associated with mutism after posterior fossa surgery in children. Neurosurgery. 1998; 42:253–7.
Hoksbergen I, Pickut BA, Mariën P, Slabbynck H, Kunnen J, De DeynPP. SPECT findings in an unusual case of visual hallucinosis. J Neurol. 1996;243:594–8.
Trimble MH. Psychopathology of frontal lobe syndromes. Sem Neurol. 1990;10:287–94.
Levy RDubois. Apathy and the functional anatomy of the prefrontal cortex-basal ganglia circuits. Cerebr Cortex. 2005;16: 916–28.
Mariën P, Engelborghs S, Fabbro F, De DeynPP. The lateralized linguistic cerebellum: A review and a new hypothesis. Brain Lang. 2001;79:580–600.
Germano A, Baldari S, Caruso G, Caffo M, Montemagno G, Cardia E, et al. Reversible cerebral perfusion alterations in children with transient mutism after posterior fossa surgery. Child Nerv Syst. 1998;14:114–19.
Mariën P, Verhoeven J, Engelborghs S, Rooker S, Pickut BA, De DeynPP. A role for the cerebellum in motor speech planning: Evidence from foreign accent syndrome. Clin Neurol Neurosurg. 2006;108:512–22.
Ersahin Y, Yararbas U, Duman Y, Mutluer S. Single photon emission tomography following posterior fossa surgery in patients with and without mutism. Child Nerv Syst. 2002;18: 318–25.
Gerrard P, Bradshaw D, Jäger HR, Thompson AJ, Losseff N, Playford D. Cognitive dysfunctions after isolated brain stem insult. An underdiagnosed cause of long-term morbidity. J Neurol Neurosurg Psychiatry. 2002;73: 191–4.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baillieux, H., De Smet, H.J., Lesage, G. et al. Neurobehavioral alterations in an adolescent following posterior fossa tumor resection. Cerebellum 5, 289–295 (2006). https://doi.org/10.1080/14734220601009606
Issue Date:
DOI: https://doi.org/10.1080/14734220601009606