Abstract
Introduction
We report the first case of an intraoperative radiotherapy (IORT) in a patient with recurrent glioblastoma multiforme (GBM) who was followed up with a novel magnetic resonance imaging (MRI) method—23Na-MRI—in comparison to a standard contrast-enhanced 1H-MRI and 18F-FET-PET.
Methods
A 56-year-old female patient with diagnosed GBM in July 2012 underwent tumor resection, radiochemotherapy, and three cycles of chemotherapy. After a relapse, 6 months after the initial diagnosis, an IORT was recommended which was performed in March 2013 using the INTRABEAM system (Carl Zeiss Meditec AG, Germany) with a 3-cm applicator and a surface dose of 20 Gy. Early post-operative contrast-enhanced and 1-month follow-up 1H-MRI and a 18F-FET-PET were performed. In addition, an IRB-approved 23Na-MRI was performed on a 3.0-T MR scanner (MAGNETOM TimTrio, Siemens Healthcare, Germany).
Results
After re-surgery and IORT in March 2013, only a faint contrast enhancement but considerable surrounding edema was visible at the medio-posterior resection margins. In April 2013, new and progressive contrast enhancement, edema, 23Na content, and increased uptake in the 18F-FET-PET were visible, indicating tumor recurrence. Increased sodium content within the area of contrast enhancement was found in the 23Na-MRI, but also exceeding this area, very similar to the increased uptake depicted in the 18F-FET-PET. The clearly delineable zone of edema in both examinations exhibits a lower 23Na content compared to areas with suspected proliferating tumor tissue.
Conclusion
23Na-MRI provided similar information in the suspicious area compared to 18F-FET-PET, exceeding conventional 1H-MRI. Still, 23Na-MRI remains an investigational technique, which is worth to be further evaluated.
Similar content being viewed by others
Introduction
Among primary brain tumors, glioblastoma multiforme (GBM) remains one of the most frequent, most aggressive, and most fatal tumors with a median survival of about 14 months [1]. The current multimodal therapy approach includes a combination of tumor resection, radiochemotherapy, and adjuvant chemotherapy. Nevertheless, local tumor recurrence observed within a distance of 2–3 cm to the initial lesion represents the main cause for (lethal) clinical worsening. A uniform therapy concept of recurrent GBM is lacking and also various second-line therapy strategies do not considerably improve survival times ranging from 3 to 4 months [2]. One approach for the treatment of pre-irradiated and re-resectable recurrent GBM is the application of intraoperative radiotherapy (IORT) [3]. Specifically in the recurrent setting, when re-irradiation is only feasible in dose- and volume-reduced schemes to avoid complications, the delivery of a local dose of radiotherapy with steep gradients to healthy tissues may be an approach to prolong the time to re-intervention.
However, any dose escalation strategy bears the risk of brain necrosis, which requires short follow-up intervals and suitable imaging strategies. Specifically, the latter are intensively discussed in the recurrent setting, where salvage therapies (such as IORT or antiangiogenic substances) are applied [4, 5]. Clinical imaging concepts of GBM are mainly based on contrast-enhanced magnetic resonance imaging (MRI), which is of questionable use in the post-operative and post-radiotherapy setting [6].
Up to now, there is no sufficient morphological distinction between tumor relapse and post-treatment injured brain tissue. Novel diagnostic options include functional MR imaging, such as diffusion-weighted imaging (DWI) or MR spectroscopy and 18F-fluoro-ethyl-tyrosin-positron-emissions-tomography (18F-FET-PET), which appears to be a specifically good discriminator of the abovementioned morphological changes. First studies even discuss 18F-FET-PET to be superior to MRI [7, 8] in the situation of recurrent tumors.
Over the past few years, the potential of 23Na-MRI was rediscovered and progressively tried to be implemented in a clinical setting [9]. In contrast to standard MRI, which is based on the visualization of 1H, 23Na-MRI uses the signal of tissue sodium (23Na)—expressed as tissue sodium concentration (TSC). Recent studies found an up to threefold increase in TSC in human strokes [10] allowing monitoring of the progression of stroke pathophysiology [11]. In different brain tumors, Ouwerkerk et al. described increased sodium concentrations relative to normal brain structures, which are likely a reflection of an altered ion homeostasis. This is most likely due to an increase in both extracellular volume fraction as well as intracellular sodium [12]. Furthermore, Nagy et al. and Cameron II et al. have shown that reduced (Na+/K+) adenosine triphosphatase activity and altered Na+/H+ exchange kinetics, which lead to an increased intracellular sodium, are associated with malignancy [12, 13]. Thulborn et al. discussed the method as a potential therapy-monitoring tool [14, 15] which could be easily transferred to other organs [16].
The purpose of our study was to evaluate the first case of an IORT in a patient with recurrent GBM who was followed up with a recently introduced magnetic MRI method—23Na-MRI—in comparison to a standard contrast-enhanced 1H-MRI and 18F-FET-PET.
Material and methods
Clinical and imaging history
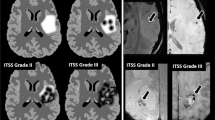
This case report describes the clinical course of a 56-year-old female patient who was diagnosed with GBM in July 2012 after several episodes of gait instability and progressive left-sided hemiparesis. Despite gross tumor resection, radiochemotherapy and three cycles of standard adjuvant chemotherapy (150 mg/m2/5-day cycle temozolomide in a 28-day scheme), she relapsed 6 months after the initial diagnosis. Due to her young age, a good clinical performance status, a circumscribed, well-accessible local relapse, and an unfavorable histology with a demethylated MGMT promoter, the interdisciplinary tumor board recommended re-operation with IORT. In March 2013, surgery was performed and IORT was applied using the INTRABEAM® system (Carl Zeiss Meditec AG, Germany) with a 3-cm applicator and a surface dose of 20 Gray (Gy). Routine early post-operative contrast-enhanced 1H-MRI was performed (Fig. 1a, b) according to the local guidelines, showing post-operative changes only in a small area of contrast enhancement at the medio-posterior margin at best. The 1-month follow-up MRI (Fig. 2a–d) presented new and progressive contrast-enhancing areas at the resection margins, prompting the tumor board to recommend 18F-FET-PET imaging which confirmed a second recurrence (Fig. 2d). Due to the limited therapeutic options and the absence of clinical symptoms, the patient was entering a tightly scheduled follow-up with MRI and placed on a metronomic therapy with daily temozolomide (20 mg/m2 bid) and Celebrex (celecoxib) [17].
The follow-up examination with 1H-MRI (a, c), 23Na-MRI (b), and 18F-FET-PET (d) showed a worsening situation with progressive contrast enhancement, but decreasing edema (arrowheads). 23Na-MRI shows an increased TSC posteriorly, relatively similar to the 18F-FET-PET (arrows). {a Fusion of the T1w post CM 1H-images and the color-encoded 23Na-image}
Three months after re-surgery and IORT (7/2013), MRI revealed a progressive T2-FLAIR edema (Fig. 3d) and multiple progressive contrast-enhancing areas around the cavity and, most concerning, also a new contrast-enhancing lesion in the lateral aspect of the brain stem in the still asymptomatic patient. Table 1 shows a timeline of events. Although the patient was promptly admitted to hypofractionated radiotherapy of the brain stem lesion and the former resection cavity (brain stem lesion, 45 Gy in 15 fractions; resection cavity, 36 Gy in 15 fractions), her condition rapidly deteriorated 1 day before receiving the last fraction and she finally deceased 6 months after re-surgery/IORT (14 months after the initial diagnosis).
23Na-MR imaging
Institutional review board approval and informed consent was obtained in accordance to the Declaration of Helsinki in this prospective study. The patient was examined on a clinical, whole-body 3.0-Tesla MR scanner (MAGNETOM TimTrio 32 × 102, Siemens Healthcare, Germany), positioned supine, headfirst on the table. For signal reception, an 8-channel, double-tuned 1H-/23Na- birdcage head coil (Rapid Biomedical, Germany) was used. The 1H-protocol consisted of standard morphological T2w, T1w, DWI sequences with the application of gadolinium-based contrast agent (Dotarem®, Guerbet, France). For 23Na-imaging, a 3D density-adapted projection reconstruction sequence [18], with the following sequence parameters—optimized for 23Na-imaging—was acquired: echo time = 0.2 ms, repetition time = 100 ms, projections = 6000, nominal spatial resolution = 4 × 4 × 4 mm3, and acquisition time = 10 min. The offline reconstructed 23Na-images were matched with the 1H-morphological MP-Rage images using the statistical parametric mapping toolbox (SPM8, The Wellcome Trust Centre for Neuroimaging, London) for MATLAB (R2010a, The MathWorks Inc., Natick, MA, USA).
Sodium tissue concentration is given semi-quantitatively as a signal-to-noise-ratio (SNR). The SNR was calculated as signal of the region-of-interests (manually drawn in the 1H-morphological images and copied onto the 23Na-image—except for the suspicious areas with visibly increased 23Na-content) divided by the standard deviation measured in a 2-cm2 circular ROI in air. ROIs were drawn in depictable tumor-free white matter (WM) on the right frontal side, normal appearing WM in the frontal and occipital left hemisphere, within areas of edema and suspicious, partially contrast-enhancing areas at the resection margin. Descriptive statistics but no further statistical testing was performed due to the character of a case report.
Results
After re-surgery and IORT in March 2013, only a faint contrast enhancement (Fig. 1a) but considerable surrounding edema (Fig. 1b) is visible at the medio-posterior resection margins. It is unclear whether the contrast enhancement represents remaining tumor or injured brain tissue. In the short-term follow-up (April 2013), new and progressive contrast enhancement, edema, 23Na content, and increased uptake in the 18F-FET-PET were visible (Fig. 2a–d), indicating tumor recurrence. In the performed 18F-FET-PET, the increased uptake could be delineated exemplarily in the posterior parts adjacent to the margins, confirming the relapsing tumor. Increased sodium content within the area of contrast enhancement was found in the 23Na-MRI, but also exceeding this area, very similar to the 18F-FET-PET. Imaging in July 2013 presented a vast worsening with increased contrast enhancement, edema, and 23Na-content (Figs. 3 and 4). The clearly delineable zone of edema in both examinations exhibits a lower 23Na-content compared to areas with suspected proliferating tumor tissue (Figs. 2 and 3).
Discussion
We here report the first 23Na-MR imaging study on a patient that underwent salvage IORT for recurrent GBM. Locally intensified therapy approaches such as IORT, chemotherapy wafers, convection-enhanced delivery, and brachytherapy are believed to improve survival in GBM [3, 19]. However, although there is an increasing use of these techniques, little is known on the induced morphological changes in conventional imaging studies. Our center is currently running the first phase I/II study to investigate maximum tolerated doses of IORT in primary GBM (INTRAGO-Intraoperative Radiotherapy for Glioblastoma; NCT02104882), and we are thus specifically committed to distinguish post-irradiation changes (and complications such as necrosis) from actual progressive disease. One standardized approach is the application of the updated Response Assessment in Neuro-Oncology Criteria (RANO criteria) [20]. However, these criteria do not take into account the growing application of local therapies (such as IORT) and are of questionable significance in patients undergoing antiangiogenic therapy [21].
Here, MR spectroscopy may offer an increased diagnostic confidence and the possibility to differentiate the tissue content by assessing its metabolic components [22]. This technique is unfortunately challenging and prone to technical failure. Furthermore, it is not possible or very time-consuming to include the complete resection margin within a single-voxel MRS technique. Consequently, new diagnostic alleys as the extremely potential 18F-FET-PET, which seems favorable, compared to standard contrast-enhanced MRI [7] are up for discussion. One of its drawbacks is the quite expensive and not widely available tracer. As 18F-FET-PET imaging is not available on a daily routine in every medical center that treats GBM, cost-effective alternatives are thus warranted.
In our report, 23Na-MRI is used in the post-interventional follow-up in comparison to 18F-FET-PET for the first time, showing relatively similar information and, in addition, exceeding the enhancement pattern of conventional 1H-MRI. 23Na-MRI offers a potential for tumor imaging and (therapy) follow-up, which on the one hand was shown in animal studies [23–27] for different tumor entities, but also in first human studies with lung cancer [28] and GBM [29]. In their feasibility study, Laymon et al. [29] have shown that [18F]fluorothymidine (18F-FLT) PET and 23Na-MRI at 3.0 T have independently detected changes of GBM tissue under therapy which may be providing complementary information in terms of tumor progression. Still, 23Na-MRI remains an investigational technique, which is worth to be further evaluated.
In conclusion, our study demonstrates that non-invasive 23Na-MRI shows similar information in comparison to 18F-FET-PET. If we can verify our first results in more patients, there might be hope to allow discriminating tumor progression and pseudoprogression in the future.
References
Stupp R et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352(10):987–996
Park JK et al (2010) Scale to predict survival after surgery for recurrent glioblastoma multiforme. J Clin Oncol 28(24):3838–3843
Giordano F et al (2014) Intraoperative radiotherapy (IORT)—a resurrected option for treating glioblastoma? Transl Cancer Res 3(1):94–105
Weller M et al (2013) Standards of care for treatment of recurrent glioblastoma—are we there yet? J Neurooncol 15(1):4–27
Kreisl TN et al (2009) Phase II trial of single-agent bevacizumab followed by bevacizumab plus irinotecan at tumor progression in recurrent glioblastoma. J Clin Oncol 27(5):740–745
Brandsma D et al (2008) Clinical features, mechanisms, and management of pseudoprogression in malignant gliomas. Lancet Oncol 9(5):453–461
Galldiks N et al (2012) Assessment of treatment response in patients with glioblastoma using O-(2-18F-fluoroethyl)-l-tyrosine PET in comparison to MRI. J Nucl Med Off Publ Soc Nucl Med 53(7):1048–1057
Gotz I, Grosu AL (2013) [18F]FET-PET imaging for treatment and response monitoring of radiation therapy in malignant glioma patients—a review. Front Oncol 3:104
Haneder S, et al (2013) Sodium (23Na)-imaging as therapy monitoring in oncology—future prospects. MAGNETOM Flash. 2 (ISMRM edition)(52):72–77
Maudsley AA, Hilal SK (1984) Biological aspects of sodium-23 imaging. Br Med Bull 40(2):165–166
Thulborn KR et al (2005) Sodium MR imaging of acute and subacute stroke for assessment of tissue viability. Neuroimaging Clin N Am 15(3):639–653, xi–xii
Nagy I et al (1983) Correlation of malignancy with the intracellular Na+:K+ ratio in human thyroid tumors. Cancer Res 43(11):5395–5402
Cameron IL et al (1980) Intracellular concentration of sodium and other elements as related to mitogenesis and oncogenesis in vivo. Cancer Res 40(5):1493–1500
Ouwerkerk R et al (2003) Tissue sodium concentration in human brain tumors as measured with 23Na MR imaging. Radiology 227(2):529–537
Thulborn KR et al (2009) Quantitative sodium MR imaging and sodium bioscales for the management of brain tumors. Neuroimaging Clin N Am 19(4):615–624
Danisch M et al (2014) Bilateral 23Na MR imaging of the breast and quantification of sodium concentration. Z Med Phys 24(1):65–72
Stockhammer F et al (2010) Continuous low-dose temozolomide and celecoxib in recurrent glioblastoma. J Neurooncol 100(3):407–415
Nagel AM et al (2009) Sodium MRI using a density-adapted 3D radial acquisition technique. Magn Reson Med Off J Soc Magn Reson Med Soc Magn Reson Med 62(6):1565–1573
Brem H et al (1995) Placebo-controlled trial of safety and efficacy of intraoperative controlled delivery by biodegradable polymers of chemotherapy for recurrent gliomas. The polymer-brain tumor treatment group. Lancet 345(8956):1008–1012
Wen PY et al (2010) Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol 28(11):1963–1972
Hutterer M et al (2011) O-(2-18F-fluoroethyl)-l-tyrosine PET predicts failure of antiangiogenic treatment in patients with recurrent high-grade glioma. J Nucl Med 52(6):856–864
Ryken TC, et al (2014) The role of imaging in the management of progressive glioblastoma: a systematic review and evidence-based clinical practice guideline. Journal of Neuro-oncology
Kline RP et al (2000) Rapid in vivo monitoring of chemotherapeutic response using weighted sodium magnetic resonance imaging. Clin Cancer Res Off J Am Assoc Cancer Res 6(6):2146–2156
Babsky AM et al (2005) Application of 23Na MRI to monitor chemotherapeutic response in RIF-1 tumors. Neoplasia 7(7):658–666
Sharma R et al (2005) Rapid in vivo taxotere quantitative chemosensitivity response by 4.23 Tesla sodium MRI and histo-immunostaining features in N-methyl-N-nitrosourea induced breast tumors in rats. Cancer Cell Int 5:26
Schepkin VD et al (2006) Sodium and proton diffusion MRI as biomarkers for early therapeutic response in subcutaneous tumors. Magn Reson Imaging 24(3):273–278
Schepkin VD et al (2006) Proton and sodium MRI assessment of emerging tumor chemotherapeutic resistance. NMR Biomed 19(8):1035–1042
Henzler T et al (2012) Imaging of tumor viability in lung cancer: initial results using 23Na-MRI. RoFo: Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin 184(4):340–344
Laymon CM et al (2012) Combined imaging biomarkers for therapy evaluation in glioblastoma multiforme: correlating sodium MRI and F-18 FLT PET on a voxel-wise basis. Magn Reson Imaging 30(9):1268–1278
Ethical standards and patient consent
We declare that all human studies have been approved by the Institutional Review Board and Ethics Commitee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. We declare that all patients gave informed consent prior to inclusion in this study.
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haneder, S., Giordano, F.A., Konstandin, S. et al. 23Na-MRI of recurrent glioblastoma multiforme after intraoperative radiotherapy: technical note. Neuroradiology 57, 321–326 (2015). https://doi.org/10.1007/s00234-014-1468-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-014-1468-2