Abstract
Objectives
To assess whether 1H-MRS may be useful to reinforce the radiological suspicion of PCNSL.
Methods
In this retrospective study, we included 546 patients with untreated brain tumours in which single-voxel spectroscopy at TE 30 ms and 136 ms had been performed. The patients were split into two subgroups: “training set” and “test set.” Differences between PCNSL and five other types of intracranial tumours were assessed in the test set of patients using the Mann-Whitney U nonparametric test and cut-off values for pair-wise comparisons defined by constructing receiver operating characteristic curves. These thresholds were used to construct classifiers for binary comparison between PCNSL and non-PCNSL. The performance of the obtained classifiers was assessed in the independent test set of patients.
Results
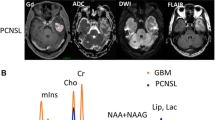
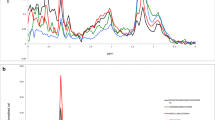
Significant differences were found between PCNSL and the other groups evaluated. All bilateral comparisons performed in the test set obtained accuracy values above 70 % (71–89 %). Lipids were found to be useful to discriminate between PCNSL and glioblastoma/metastasis at short TE. Myo-inositol resonance was found to be very consistent for discriminating between PCNSL and astrocytomas at short TE.
Conclusions
1H-MRS is useful to reinforce diagnostic suspicion of PCNSL on MRI.
Key Points
• 1 H-MRS can be used to reinforce the diagnostic suspicion of PCNSL.
• Lipids can be used to discriminate between PCNSL and GB/MET.
• Myo-inositol resonance can be used to discriminate between PCNSL and astrocytomas.





Similar content being viewed by others
Abbreviations
- PCNSL:
-
Primary central nervous system lymphoma
- MEN:
-
Meningioma
- LGA:
-
Low-grade astrocytoma
- AA:
-
Anaplastic astrocytoma
- GB:
-
Glioblastoma
- MET:
-
Metastases
- Glx:
-
Glutamate/glutamine
- ALA:
-
Alanine
- TAU:
-
Taurine
- Cr:
-
Creatine
- Cho:
-
Choline
- mIns:
-
Myo-inositol
References
Dolecek TA, Propp JM, Stroup NE, Kruchko C (2012) CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2005–2009. Neuro-Oncol 14:v1–v49
Hunt MA, Jahnke K, Murillo TP, Neuwelt EA (2006) Distinguishing primary central nervous system lymphoma from other central nervous system diseases: a neurosurgical perspective on diagnostic dilemmas and approaches. Neurosurg Focus 21:E3
Hashemi-Sadraei N, Peereboom DM (2010) Chemotherapy in newly diagnosed primary central nervous system lymphoma. Ther Adv Med Oncol 2:273–292
Graber JJ, Omuro A (2011) Primary central nervous system lymphoma: is there still a role for radiotherapy? Curr Opin Neurol 24:633–640
Haldorsen IS, Kråkenes J, Krossnes BK, Mella O, Espeland A (2009) CT and MR imaging features of primary central nervous system lymphoma in Norway, 1989–2003. AJNR Am J Neuroradiol 30:744–751
Majós C, Alonso J, Aguilera C et al (2002) Adult primitive neuroectodermal tumor: proton MR spectroscopic findings with possible application for differential diagnosis. Radiology 225:556–566
Van den Boogaart A (1997) Quantitative data analysis of in vivo MRS data sets. Magn Reson Chem 35:S146–S152
Majós C, Bruna J, Julià-Sapé M et al (2011) Proton MR spectroscopy provides relevant prognostic information in high-grade astrocytomas. AJNR Am J Neuroradiol 32:74–80
Hochberg Y, Tamhane AC (1987) Multiple comparison procedures. Wiley, New York
Obuchowski NA (2003) Receiver operating characteristic curves and their use in radiology. Radiology 229:3–8
Tang YZ, Booth TC, Bhogal P, Malhotra A, Wilhelm T (2011) Imaging of primary central nervous system lymphoma. Clin Radiol 66:768–777
Haldorsen IS, Espeland A, Larsson EM (2011) Central nervous system lymphoma: characteristic findings on traditional and advanced imaging. AJNR Am J Neuroradiol 32:984–992
Taillibert S, Guillevin R, Menuel C et al (2008) Brain lymphoma: usefulness of the magnetic resonance spectroscopy. J Neurooncol 86:225–229
Küker W, Nägele T, Korfel A et al (2005) Primary central nervous system lymphomas (PCNSL): MRI features at presentation in 100 patients. J Neurooncol 72:169–177
Zacharia TT, Law M, Naidich TP, Leeds NE (2008) Central nervous system lymphoma characterization by diffusion-weighted imaging and MR spectroscopy. J Neuroimaging 18:411–417
Lu SS, Kim SJ, Kim HS et al (2014) Utility of proton MR spectroscopy for differentiating typical and atypical primary central nervous system lymphomas from tumefactive demyelinating lesions. AJNR Am J Neuroradiol 35:270–277
Harting I, Hartmann M, Jost G et al (2003) Differentiating primary central nervous system lymphoma from glioma in humans using localised proton magnetic resonance spectroscopy. Neurosci Lett 342:163–166
Kuesel AC, Sutherland GR, Halliday W, Smith IC (1994) 1H MRS of high grade astrocytomas: mobile lipid accumulation in necrotic tissue. NMR Biomed 7:149–155
Kimura T, Sako K, Gotoh T, Tanaka K, Tanaka T (2001) In vivo single-voxel proton MR spectroscopy in brain lesions with ring-like enhancement. NMR Biomed 14:339–349
Opstad KS, Wright AJ, Bell BA, Griffiths JR, Howe FA (2010) Correlations between in vivo (1)H MRS and ex vivo (1)H HRMAS metabolite measurements in adult human gliomas. J Magn Reson Imaging 31:289–297
Majós C, Alonso J, Aguilera C et al (2003) Utility of proton MR spectroscopy in the diagnosis of radiologically atypical intracranial meningiomas. Neuroradiology 45:129–136
Usenius JP, Tuohimetsä S, Vainio P, Ala-Korpela M, Hiltunen Y, Kauppinen RA (1996) Automated classification of human brain tumours by neural network analysis using in vivo 1H magnetic resonance spectroscopic metabolite phenotypes. Neuroreport 7:1597–1600
Arle JE, Morriss C, Wang ZJ, Zimmerman RA, Phillips PG, Sutton LN (1997) Prediction of posterior fossa tumor type in children by means of magnetic resonance image properties, spectroscopy, and neural networks. J Neurosurg 86:755–761
Majós C, Alonso J, Aguilera C et al (2003) Proton magnetic resonance spectroscopy ((1)H MRS) of human brain tumours: assessment of differences between tumour types and its applicability in brain tumour categorization. Eur Radiol 13:582–591
Acknowledgments
The scientific guarantor of this publication is Carlos Majós MD, PhD. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. This study has received funding in part by MARESCAN (Ministerio de Educación y Ciencia SAF 2011-23870), and by CIBER-BBN, which is an initiative funded by the VI National R&D&I Plan 2008–2011, Iniciativa Ingenio 2010, Consolider Program, CIBER Actions, and financed by the Instituto de Salud Carlos III, with assistance from the European Regional Development Fund, Spain. One of the authors has significant statistical expertise. This retrospective study was included in a research project that had local ethics committee approval. Written informed consent for routine MR imaging studies was obtained from all patients in this study. Some study subjects or cohorts have been previously reported in:
Majós C, Julià-Sapé M, Alonso J, et al. (2004) Brain Tumor Classification by Proton MR Spectroscopy: Comparison of Diagnostic Accuracy at Short and Long TE. AJNR Am J Neuroradiol 25:1696-1704
Majós C, Aguilera C, Alonso J, et al. (2009) Proton MR Spectroscopy Improves Discrimination between Tumor and Pseudotumoral Lesion in Solid Brain Masses. AJNR Am J Neuroradiol 30: 544-551
Majós C, Aguilera C, Cos M, et al. (2009) In vivo proton magnetic resonance spectroscopy of intraventricular tumours of the brain. Eur Radiol 19:2049-2059
Majós C, Bruna J, Julià-Sapé M, et al. (2011) Proton MR Spectroscopy Provides Relevant Prognostic Information in High-Grade Astrocytomas. AJNR Am J Neuroradiol 32:74-80
Methodology: retrospective diagnostic or prognostic study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mora, P., Majós, C., Castañer, S. et al. 1H-MRS is useful to reinforce the suspicion of primary central nervous system lymphoma prior to surgery. Eur Radiol 24, 2895–2905 (2014). https://doi.org/10.1007/s00330-014-3308-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3308-5