Abstract
In this study we investigated the responsiveness of near-infrared spectroscopy (NIRS) recordings measuring regional cerebral tissue oxygenation (rSO2) during hypoxia in apneic divers. The goal was to mimic dynamic hypoxia as present during cardiopulmonary resuscitation, laryngospasm, airway obstruction, or the “cannot ventilate cannot intubate” situation. Ten experienced apneic divers performed maximal breath hold maneuvers under dry conditions. SpO2 was measured by Masimo™ pulse oximetry on the forefinger of the left hand. NIRS was measured by NONIN Medical’s EQUANOX™ on the forehead or above the musculus quadriceps femoris. Following apnea median cerebral rSO2 and SpO2 values decreased significantly from 71 to 54 and from 100 to 65 %, respectively. As soon as cerebral rSO2 and SpO2 values decreased monotonically the correlation between normalized cerebral rSO2 and SpO2 values was highly significant (Pearson correlation coefficient = 0.893). Prior to correlation analyses, the values were normalized by dividing them by the individual means of stable pre-apneic measurements. Cerebral rSO2 measured re-saturation after termination of apnea significantly earlier (10 s, SD = 3.6 s) compared to SpO2 monitoring (21 s, SD = 4.4 s) [t(9) = 7.703, p < 0.001, r2 = 0.868]. Our data demonstrate that NIRS monitoring reliably measures dynamic changes in cerebral tissue oxygen saturation, and identifies successful re-saturation faster than SpO2. Measuring cerebral rSO2 may prove beneficial in case of respiratory emergencies and during pulseless situations where SpO2 monitoring is impossible.
Similar content being viewed by others
1 Introduction
Since the first report of near-infrared spectroscopy (NIRS) as a noninvasive measurement for cerebral tissue oxygenation in 1977 [1], the clinical use has been constantly growing [2]. Currently NIRS is used mainly to evaluate cerebral tissue oxygen saturation (rSO2) in real-time during cardiovascular procedures, during hemorrhagic shock or in patients with subarachnoid hemorrhage [3–9]. Besides, NIRS has also become a prospective tool in terms of patient progress and outcome, development of organ dysfunction and resuscitation [10–13].
Peripheral oxygen saturation (SpO2) measured by finger pulse oximetry is an approved tool in pre-hospital and hospital settings [14]. The method is based on the light absorption of hemoglobin—non-oxygenated hemoglobin absorbs red light to a higher extent than oxygenated. In the near infrared range the effect of oxygenation on light absorption is converse. The ratio of the transmitted light at both wave-lengths [660 nm (red) and 940 nm (near infrared] provides real-time and non-invasive monitoring of arterial oxygen saturation. In contrast to SpO2, rSO2 depends mainly on venous blood [14]. In previous methodological studies a clear positive correlation between SpO2 and rSO2 has already been demonstrated [16–18]. This correlation was shown in experiments where the participants inhaled hypoxic gas mixtures consisting of reduced O2 substituted with N2 during normocapnia. Such conditions are representative for high altitude surroundings, but do not simulate clinical situations such as resuscitation, laryngospasm, bronchospasm or the “cannot ventilate cannot intubate” situation. Clinically caused hypoxia is in general accompanied by hypercapnia which is able to induce an autoregulatory blood shift into the central nervous system [19]. In these situations controlled simultaneous SpO2 and cerebral rSO2 recordings have so far only been performed in animals and not in humans due to ethical restrictions [20].
We hypothesized that voluntary apnea performed by apneic divers leads to a significant decrease of cerebral rSO2 and therefore is able to mimic clinical situations such as cardiopulmonary resuscitation, laryngospasm, bronchospasm, or the “cannot ventilate cannot intubate” situation where dynamic changes of hypoxia and hypercapnia may occur. Furthermore we hypothesized that cerebral rSO2 is better suited to identify successful re-saturation following hypoxia compared to peripheral SpO2 monitoring.
2 Materials and methods
To investigate a clinical situation of an acute decrease of SpO2 or rSO2 in volunteers, these have to be deprived of oxygen supply. This cannot be done due to ethical restrictions. Another possibility is to perform voluntary breath-hold maneuvers. Non-trained volunteers are not capable to perform breath-hold maneuvers lowering SpO2 or rSO2 [31] sufficiently to mimic dynamic hypoxia as present during cardiopulmonary resuscitation, laryngospasm, airway obstruction, or the “cannot ventilate cannot intubate” situation. Therefore experienced apneic-divers were selected for this study. The design of this study was approved by the local ethics committee of Bonn (No. 072/13).
Ten experienced apneic divers were included into the study. Participants were asked to perform their usual mental exercises (yoga and breathing exercises) for a maximum of 10 min prior to our measurements. To rule out that subsequent measurements were influenced by low carbon dioxide, hyperventilation was not allowed. Three minutes before final apnea participants stopped personal breathing exercises and were only allowed to breathe normally. Apnea was performed as long as the individual subjects were able to withstand the breathing reflex. Goal of the apneic maneuvers was to hold breath as long as possible. Measurements were performed in a lying position under dry conditions to avoid influence of hydrostatic pressure on assumed reactive peripheral vasoconstriction mediated by hypoxia.
Before, during and after apnea heart rate was measured by a continuous five-lead electrocardiogram (ECG) (Dräger monitor system: Infinity® M540 Monitor and Infinity M500 Docking Station, Lübeck, Germany). SpO2 was measured on the left forefinger by a Dräger-integrated Masimo monitoring system (SHP ACC MCABLE-Masimo Set, OEM partners of Dräger Medical AG&Co.KG, Lübeck, Germany). Cerebral oxygen saturation (cerebral rSO2) was measured by a stand-alone NONIN monitor through NIRS technology (NONIN Medical’s EQUANOX™, Model 7600 Regional Oximeter System, Plymouth, USA). NIRS diodes (EQUANOX Advance™ Sensor, Model 8004CA, suited for measuring cerebral and somatic oxygen-saturation) were placed on the right forehead above the eyebrow and to the right of the midsaggital sulcus (locus frontopolar 2). EQUANOX Advance utilizes four wavelengths (between 720 nm and 880 nm) of light to measure the balance of oxygenated and deoxygenated hemoglobin. ECG, SpO2 and cerebral rSO2 were continuously recorded, digitalized and stored on a hard drive of a laptop computer for offline analysis. SpO2 and cerebral rSO2 recording systems were set to their normal clinical sampling rates (SpO2 1 s−1 and cerebral rSO2 1 s−1). Monitors displaying vital parameters were invisible for all volunteers.
The internal clocks of the EQUANOX and M540 monitors were reset to exactly the same time prior to each experiment (accuracy 1 s). Synchronization between the EQUANOX and M540 signals was then performed offline.
To evaluate methodological differences between cerebral rSO2 and SpO2 measurements peripheral NIRS measurements were investigated in a new set of experiments as well (n = 7). The second set of experiments was performed 1 month later to warrant independent experimental conditions. As SpO2 recordings were performed on the left forefinger tip it would have been optimal to measure NIRS signals from a neighboring finger. This however is technically infeasible. Alternatively, the NIRS sensor could be placed on the forearm. However, preliminary tests showed that NIRS recordings displayed high variability in case of small local alterations. This may be caused by the dense subcutaneous venous plexus in this area. Therefore peripheral diodes were finally placed above the middle of the musculus quadriceps femoris (NIRSperipheral). We recorded SpO2 from the left forefinger, which is behind the branching of aorta and brachiocephalic trunk. If changes in blood flow following hypoxia lead to differential vasoconstriction and vasodilatation with preferential blood supply of the CNS (cerebral autoregulation), the assumed peripheral vasoconstriction should influence the perfusion of the left fingers and the legs in a comparable manner. In this second set of experiments (n = 7) blood pressure was recorded continuously from the tips of finger 3 and 4 by the Infinity® CNAP™ SmartPod® system (Dräger Medical AG&Co.KG, Lübeck, Germany) in addition to NIRSperipheral.
2.1 Data analysis methods
Total decrease of cerebral rSO2 and SpO2 measurements during apnea was tested for significance. Because the distribution of measurement differences in NIRS values differed significantly from a normal distribution (Shapiro–Wilk W = 0.834, p = 0.038), the total decrease was tested using two-tailed Wilcoxon signed rank tests. The Shapiro–Wilk test was preferred over alternative formal tests of normality because of its higher statistical power in samples smaller than n = 50.
The start point of rSO2 and SpO2 decrease during apnea was defined as a drop of >2 % compared to stable pre-apneic measurements followed by a monotonic decreasing time-course. The start of increasing cerebral rSO2 and SpO2 was defined by a change of monotonically decreasing to steadily increasing values after onset of breathing. Mean differences of time delays for cerebral rSO2 versus SpO2 decrease following apnea and the corresponding increases following restart of respiration were investigated using two-tailed paired t tests. There were no indications of violations of distributional assumptions underlying the t test. As before, the Shapiro–Wilk normality test was applied to test for Gaussian distribution of the data (decrease: W = 0.987, p = 0.990; increase: W = 0.958, p = 0.757).
In a consecutive experiment we investigated time delays in NIRSperipheral compared to SpO2 decrease following apnea and the corresponding increases following restart of respiration. Again, Shapiro–Wilk normality test did not indicate significant violations of the assumptions underlying two-tailed paired t tests (decrease: W = 0.832, p = 0.084; increase: W = 0.828, p = 0.077). Furthermore, the differences in SpO2 time delays between the first and second experiment were tested for significance using two-tailed t tests. Shapiro–Wilk normality tests and Fisher’s F tests did not indicate significant violations of the assumptions underlying two-tailed t tests.
In addition, we compared the mean blood pressure at the beginning and end of apnea. This difference was investigated using two-tailed paired t tests after checking for violation of the distributional assumptions (Shapiro–Wilk W = 0.976, p = 0.936).
The correlation analyses were performed for the pooled SpO2 and cerebral rSO2 values of all participants. Prior to correlation analyses, the values were normalized by dividing them by the individual means of stable pre-apneic measurements. This normalization was carried out to control for inter-individual baseline differences of rSO2 values before pooling the data for analysis.
To prevent spurious correlations due to deep breath exercises (although hyperventilation was not allowed, deep breath exercises influenced cerebral saturation by increasing the intrathoracic pressure at the beginning of apnea), the correlation analysis was only based on normalized rSO2 and SpO2 values unaffected by these influences.
The statistical association between cerebral rSO2 and SpO2 measurements during apnea were assessed using both Pearson’s correlation and Spearman’s rank correlation coefficient. The corresponding confidence intervals were evaluated using nonparametric bootstrapping (10,000 bootstrap samples per confidence interval).
In order to correlate SpO2, cerebral rSO2 and NIRSperipheral from different subjects and from two sets of experiments we normalised the individual apnoea duration to 100 % and standardised the respective SpO2, cerebral rSO2 and NIRSperipheral to the baseline value (set to 100 %) of each subject before start of breath hold (Fig. 4).
3 Results
The participants age ranged between 29 and 61 years (mean age of 44 years). Nine men and one woman (participant 3) were studied (see Table 1).
Following apnea, median cerebral rSO2 values decreased from a baseline level of 71 % (range 85–55) to 54 % (range 74–24) at the end of apnea (U = −2.807, exact p = 0.002). There was also a significant decrease in median SpO2 measurements from 100 % (range 100–98) to 65 % (range 90–52) at the end of apnea (U = −2.807, exact p = 0.002). In this set of experiments the average apnea time was 284.5 s (SD = 45) and minimal heart rate was 49 (SD = 14).
Figure 1a, b displays original recordings of simultaneous cerebral rSO2 and SpO2 measurements during apnea in 2 different participants. In both participants’ cerebral rSO2 and SpO2 revealed comparable kinetics of decreasing values during apnea. To further support these individual observations a correlation analysis between cerebral rSO2 and SpO2 was performed for the data of all participants (n = 10; Fig. 2). Normalized cerebral rSO2 and SpO2 values revealed a high positive correlation during apnea, indicating an almost perfect linear relationship between both parameters even in dynamic circumstances.
Raw data of two participants. a Total apnea-time was 316 s. Subject exhibited an earlier decrease in SpO2 than in cerebral rSO2. b Total apnea-time was 349 s. This subject developed the lowest HR (<40 beats/min for over 1 min) and the longest time-delay between rSO2 and SpO2 signal increase following re-saturation (23 s)
The Pearson correlation of 0.893 (95 % CI 0.882–0.902) revealed a strong linear relationship between normalised cerebral rSO2 and SpO2. Correspondingly, Spearman’s rank correlation coefficient was 0.741 (95 % CI 0.716–0.765). Due to high inter-individual variability of baseline cerebral rSO2 values ranging from 85 to 55 %, the correlation coefficients of raw (i.e., non-normalized) cerebral rSO2 and SpO2 values were only 0.589 (95 % CI 0.552–0.622) and 0.413 (95 % CI 0.375–0.449) for the Pearson and the Spearman correlation analysis, respectively.
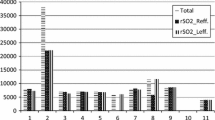
Figure 3a displays the mean time delay between beginning of apnea and decrease in cerebral rSO2 versus SpO2 values. Cerebral rSO2 values decreased after a mean time delay of 175 s (SD = 50 s) whereas SpO2 values decreased significantly earlier after a mean time delay of 134 s [SD = 29 s; t(9) = 2.865, p = 0.019, r2 = 0.477].
a Mean time delay between beginning of apnea and decrease of cerebral rSO2 versus SpO2 values [n = 10, t(9) = 2.865, p = 0.019, r2 = 0.477]. b Mean time delay between beginning of apnea and decrease of NIRSperipheral versus SpO2 values [n = 7, t(6) = 4.869, p = 0.003, r2 = 0.798]. c Mean time delay between restart of respiration and an increase of cerebral rSO2 versus SpO2 values [n = 10, t(9) = 7.703, p < 0.001, r2 = 0.868]. d Mean time delay between restart of respiration and an increase of NIRSperipheral versus SpO2 values [n = 7, t(6) = 0.631, p = 0.551, r2 = 0.062]. Error bars indicate standard error of the mean. a–d Time delays in SpO2 decrease and increase between the first and the second experiment were not significantly different [desaturation: t(15) = 0.574, p = 0.574, r2 = 0.022; re-saturation: t(15) = 2.028, p = 0.061, r2 = 0.215]
After restart of respiration, cerebral rSO2 values increased after a mean delay of only 10 s (SD = 4 s), whereas SpO2 values increased significantly later with a mean latency of 21 s [SD = 4 s; t(9) = 7.703, p < 0.001, r2 = 0.868] (Fig. 3c).
In a second independent experiment performed 1 month later we investigated the differences in time delays (de- and re-saturation) of peripheral NIRS values measured above the musculus quadriceps femoris (NIRSperipheral) and SpO2 values during apnea. In this set of experiments the average apnea time was 186.6 s (SD = 31), median SpO2 decreased from 98 % (range 100–98) to 81 % (range 94–67). (U = −2.366, exact p = 0.016) and the average minimal heart rate was 69 bpm (SD = 13).
NIRSperipheral values decreased after a mean time delay of 39 s (SD = 13 s) whereas SpO2 values decreased after a mean time delay of 125 s (SD = 36 s) (data displayed in Fig. 3b) [t(6) = 4.869, p = 0.003, r2 = 0.798]. Figure 3d displays the mean time delays between restart of respiration and increase of NIRSperipheral and SpO2. The NIRSperipheral values increased after a mean time delay of 30 s (SD = 16 s) and SpO2 values increased after a mean delay of 27 s (SD 7 s) [t(6) = 0.631, p = 0.551, r2 = 0.062].
The additionally measured blood pressure showed an increase of mean arterial pressure (MAP) during apnea. Preapneic MAP values increased from 98 mmHg (SD = 9 mmHg) to 121 mmHg (SD = 12 mmHg) at the end of apnea [t(6) = 05.442, p = 0.002, r2 = 0.832].
While cerebral hemoglobin index [HBI = volume of hemoglobin (oxyhemoglobin + deoxyhemoglobin)] as measured by the EQUANOX 7600 stayed nearly constant during apnea (1.03 SD = 0.19 pre-apneic vs. 1.00 SD = 0.17 post-apneic), HBIperipheral decreased from 1.07 (SD = 0.22) pre-apneic to 0.94 (SD = 0.15) at the end of apnea.
4 Discussion
We could demonstrate that voluntary apnea performed by apneic divers mimicking respiratory emergencies or cardiopulmonary resuscitation leads to a significant decrease of cerebral rSO2 and was highly correlated with decreasing SpO2 values. Furthermore we could show that cerebral rSO2 is better suited to identify successful re-saturation following hypoxia compared to peripheral SpO2 monitoring.
To explore whether the observed time delays of measured de- or resaturation between cerebral rSO2 and SpO2 were caused by the different techniques of signal processing (instead of physiological processes), we performed additional experiments to investigate NIRS recordings above peripheral tissue. As mentioned in Sect. 2, the EQUANOX 7600 was equipped with specific diodes, allowing to measure somatic as well as cerebral rSO2. Interestingly, NIRSperipheral dropped significantly earlier than SpO2. This may be regarded as a sign for reduced blood perfusion in the monitored tissue. We speculate that peripheral vasoconstriction occurs before a decrease in arterial oxygen saturation—visualized by SpO2—is measureable. We believe that peripheral vasoconstriction leading to a decrease in oxygen delivery may result in decreased tissue oxygenation as measured by NIRSperipheral. This may explain why NIRSperipheral demonstrates desaturation prior to SpO2 as can be seen in Fig. 4.
Displayed are normalised SpO2, cerebral rSO2 and NIRSperipheral values. To equilibrate individual variations in apnea time, all apnea times were standardised to 100 %. Thus the variations in the three plotted parameters are assigned to the relative apnea times. Baseline values measured prior to apnea were defined as 100 %
From the NIRS signal a hint for vasoconstriction may be deduced by taking the hemoglobin index [HBI = volume of hemoglobin (oxyhemoglobin + deoxyhemoglobin)] as measured by the EQUANOX 7600 device into account. While cerebral HBI stayed nearly constant during apnea HBIperipheral decreased from 1.07 pre-apneic to 0.94 at the end of apnea.
During re-saturation significant differences in time delays between both measurements (NIRSperipheral vs. SpO2) could not be seen. It is therefore unlikely that the observed time delay differences in de- or re-saturation are due to the underlying signal processing techniques (temporal resolution, artifact algorithm etc.). The time delay between rSO2 and SpO2 values may rather be attributed to different measurement sites in the body (finger vs. cerebral) asking for physiological explanations. Physiological explanations may be seen in differential local perfusion pressure or peripheral resistance and differential local blood flow.
In general, cerebral blood flow (CBF) varies to a lower degree than that of muscle tissue. CBF is kept high even in case of low end-tidal pO2, low central venous saturation and increasing age [21–23]. Increased CBF due to cerebral autoregulation protecting the brain tissue against hypoxia may also serve as one possible explanation for the investigated time delay seen in Fig. 4 between cerebral rSO2 and SpO2 decline following apnea [24]. The effect of cerebral autoregulation has already been shown in neonates during short periods of apnea. Watkin et al. [25] have investigated cerebral rSO2 and SpO2 measurements during apnea in neonates with apnea defined as a pause in nasal flow of >4 s. The authors found that small changes in SpO2 or cerebral rSO2 showed no correlation. A close association between the two indices existed only in case of large changes in SpO2. It is tempting to speculate that cerebral autoregulation was responsible for the non-existing correlation of SpO2 and rSO2 in case of minor hypoxia and that hypoxic cerebral autoregulation is even more effective in neonates as compared to adults investigated in our study, since changes in neonatal cerebral rSO2 were only associated with SpO2 changes as high as 12 %.
Cerebral autoregulation has also been investigated in adult patients with obstructive sleep apnea (OSA) [26]. However, in case of more than 30 episodes of apnea/h, severe decreases of cerebral rSO2 were reported by NIRS recordings. It may be argued that cerebral autoregulation reached a physiological limit in these patients, resulting in cerebral desaturation. Interestingly, OSA has been reported to be accompanied by a steady increase in arterial blood pressure [27]. This is in line with our finding, that apnea in our investigations was accompanied with an increase in arterial blood pressure.
A raised total peripheral resistance (TPR) and an increased mean arterial pressure (MAP) during apnea has been reported in case of divers [28–32]. We could also measure significantly elevated MAP in the course of apnea in a subset of measurements. In addition, an increased CBF caused by an elevation of TPR and MAP combined with an increase in \({\text{P}}_{{{\text{CO}}_{2} }}\) leading to cerebral vasodilatation may serve as a physiological explanation of the observed time delay between decreasing cerebral rSO2 and SpO2 values following apnea. The influence of increased arterial \({\text{P}}_{{{\text{CO}}_{2} }}\) is further supported by experiments under hyperoxic conditions with increased inspiratory \({\text{P}}_{{{\text{CO}}_{2} }}\) (7.5 mmHg) leading to elevated CBF in test subjects [33]. Increased CBF should in theory lead to a lower arterial-venous oxygen saturation difference (avDO2), visible as higher cerebral rSO2 values. In the present study we observed that cerebral rSO2 values started to decline as soon as SpO2 levels fell below 93 % (±3 %), suggesting that a further decrease in arterial oxygen saturation cannot be compensated by the above mentioned physiological mechanisms. In this context it seems worth mentioning that cerebral autoregulation induced in breath hold divers can be demonstrated by cerebral rSO2 recordings and not by peripheral SpO2-measurements.
In a previous study by Nishiyasu et al. [28] the authors describe two groups with different physiological reactions following apnea. Subjects of the first group developed lower heart rates (<65 beats/min) and exhibited greater changes in MAP and TPR compared to a second group maintaining a minimum heart rate above 75 beats/min. Most of our participants reacted to apnea with instantaneous bradycardia (Fig. 1b). It remains unclear if a humoral response leads to the combination of TPR increase and bradycardia, or if stimulation of baroreceptors due to increased intrathoracic pressure induces reflexbradycardia. In any case, we believe that measured bradycardia seen in our participants was accompanied by elevated TPR and thereby increased CBF leading to the time delay between decreasing cerebral rSO2 and SpO2 values following apnea.
Others have tested the feasibility of NIRS to record changes in brain oxygenation induced by hypoxemia [15–18, 34–36]. However, hypoxemia was induced by application of artificial gas-mixtures simulating high altitude hypoxia. Investigations were performed for up to 4 h studying long term changes in rSO2 and SpO2 follows hypoxia [37]. Such a time-course is not representative for acute respiratory emergency situations and to the best of our knowledge investigations on cerebral rSO2 and SpO2 during acute hypoxemia in the presence of hypercapnia were still missing. Our chosen model of acute apnea corresponds to a much higher extend to the clinical situation of for example laryngospasm or resuscitation compared to the model investigating high altitude situations.
During restart of respiration, re-saturation appeared significantly earlier in cerebral rSO2 compared to SpO2 in contrast to desaturation where cerebral rSO2 values reacted with delay. As mentioned before, there was no significant delay between NIRSperipheral and SpO2 recording techniques in measuring peripheral re-saturation (Fig. 3d). Thus a delayed vasodilatation in the periphery in comparison to the brain remains as a possible explanation for the observed time delays between NIRSperipheral/SpO2 increases compared to cerebral rSO2 at the end of apnea.
Taken together, both devices (NIRS and SpO2) seem to be suited to measure dynamic changes in O2 saturation. However, NIRSperipheral appears favorable in demonstrating the onset of hypoxia whereas cerebral rSO2 seems favorable to visualize successful re-saturation when compared to traditionally measured SpO2.
The relevance of the results in the present study depends on the range of rSO2 values measured during voluntary apnea (average reduction from 71 to 54 %, however, the lowest individual value reached was 24 %). Two recently published studies [37, 38] on patients with cardiac arrest and return of spontaneous circulation (ROSC) reported of initial rSO2 values around 40 % (47.2 ± 10.7 [37]/37.2 ± 17.0 % [38]). Although apneic divers in average had higher rSO2 saturations than patients during cardiac arrest the range of recorded rSO2 values was comparable. We believe that apneic divers may serve as a model to mimic clinical situations under hypoxia in a reproducible setup.
It is worth discussing the suitability of both devices in different clinical situations. It is nearly impossible to measure O2 saturation by pulse oximetry in case of centralized minimal circulation or in case of pulseless electrical activity (PEA) [38]. NIRS monitoring is therefore well established and routinely applied during cardiac surgery or extra corporal membrane oxygenation therapy. Based on the results of our study, we believe that NIRS monitoring may also be beneficial during cardiopulmonary resuscitation or other clinical situations where dynamic changes of hypoxia and hypercapnia may occur and SpO2 monitoring is sometimes impossible. Recently published studies have favored NIRS technology for monitoring rSO2 during CPR and may perhaps also allow monitoring the efficacy of CPR [39, 40]. In our study we could show that de- and re-saturation can be monitored by NIRS in a reproducible manner. In addition, one could argue that it appears more reasonable to measure O2 saturation in the most sensible human organ towards hypoxia—the brain—compared to measuring O2 saturation in the fingertip.
5 Conclusion
During acute apnea we could reveal that NIRS is suitable to measure dynamic changes of O2 saturation reliably and quickly. NIRSperipheral appears favorable in demonstrating onset of hypoxia whereas cerebral NIRS seems favorable in measuring successful re-saturation when compared to traditionally measured SpO2. Measuring cerebral NIRS may prove beneficial in case of respiratory emergencies and during pulseless situations where SpO2 monitoring is impossible.
References
Jöbsis FF. Noninvasive, infrared monitoring of cerebral and myocardial oxygen sufficiency and circulatory parameters. Science. 1977;198:1264–7.
Scheeren TW, Schober F, Schwarte LA. Monitoring tissue oxygenation by near infrared spectroscopy (NIRS): background and current applications. J Clin Monit Comput. 2012;26:279–87.
La Monaca M, David A, Gaeta R, Lentini S. Near infrared spectroscopy for cerebral monitoring during cardiovascular surgery. Clin Ter. 2010;161:549–53.
Vernieri F, Silvestrini M, Tibuzzi F, Pasqualetti P, Altamura C, Passarelli F, Matteis M, Rossini PM. Hemoglobin oxygen saturation as a marker of cerebral hemodynamics in carotid artery occlusion: an integrated transcranial doppler and near-infrared spectroscopy study. J Neurol. 2006;253:1459–65.
Moritz S, Kasprzak P, Arlt M, Taeger K, Metz C. Accuracy of cerebral monitoring in detecting cerebral ischemia during carotid endarterectomy: a comparison of transcranial Doppler sonography, near-infrared spectroscopy, stump pressure, and somatosensory evoked potentials. Anesthesiology. 2007;107:563–9.
Hansen JH, Schlangen J, Armbrust S, Jung O, Scheewe J, Kramer HH. Monitoring of regional tissue oxygenation with near-infrared spectroscopy during the early postoperative course after superior cavopulmonary anastomosis. Eur J Cardiothorac Surg. 2013;43:e37–43.
Beilman GJ, Groehler KE, Lazaron V, Ortner JP. Near-infrared spectroscopy measurement of regional tissue oxyhemoglobin saturation during hemorrhagic shock. Shock. 1999;12:196–200.
Rhee P, Langdale L, Mock C, Gentilello LM. Near-infrared spectroscopy: continuous measurement of cytochrome oxidation during hemorrhagic shock. Crit Care Med. 1997;25:166–70.
Zweifel C, Castellani G, Czosnyka M, Carrera E, Brady KM, Kirkpatrick PJ, Pickard JD, Smielewski P. Continuous assessment of cerebral autoregulation with near-infrared spectroscopy in adults after subarachnoid hemorrhage. Stroke J Cereb Circ. 2010;41:1963–8.
Ito N, Nanto S, Nagao K, Hatanaka T, Nishiyama K, Kai T. Regional cerebral oxygen saturation on hospital arrival is a potential novel predictor of neurological outcomes at hospital discharge in patients with out-of-hospital cardiac arrest. Resuscitation. 2012;83:46–50.
Cohn SM, Nathens AB, Moore FA, Rhee P, Puyana JC, Moore EE, Beilman GJ. Tissue oxygen saturation predicts the development of organ dysfunction during traumatic shock resuscitation. J Trauma. 2007;62:44–55; discussion 54–55.
Moore FA, Nelson T, McKinley BA, Moore EE, Nathens AB, Rhee P, Puyana JC, Beilman GJ, Cohn SM. Massive transfusion in trauma patients: tissue hemoglobin oxygen saturation predicts poor outcome. J Trauma. 2008;64:1010–23.
Heringlake M, Garbers C, Käbler JH, Anderson I, Heinze H, Schön J, Berger KU, Dibbelt L, Sievers HH, Hanke T. Preoperative cerebral oxygen saturation and clinical outcomes in cardiac surgery. Anesthesiology. 2012;114:58–69.
Eichhorn JH. Pulse oximetry as a standard of practice in anesthesia. Anesthesiology. 1993;78:423–6.
Shah N, Trivedi NK, Clack SL, Shah M, Shah PP, Barker S. Impact of hypoxemia on the performance of cerebral oximeter in volunteer subjects. J Neurosurg Anesthesiol. 2000;12:201–9.
Ricci M, Lombardi P, Schultz S, Galindo A, Coscarella E, Vasquez A, Rosenkranz E. Near-infrared spectroscopy to monitor cerebral oxygen saturation in single-ventricle physiology. J Thorac Cardiovasc Surg. 2006;131:395–402.
Kusaka T, Isobe K, Nagano K, Okubo K, Yasuda S, Kondo M, Itoh S, Hirao K, Onishi S. Quantification of cerebral oxygenation by full-spectrum near-infrared spectroscopy using a two-point method. Comp Biochem Physiol A Mol Integr Physiol. 2002;132:121–32.
Ainslie PN, Ogoh S. Regulation of cerebral blood flow in mammals during chronic hypoxia: a matter of balance. Exp Physiol. 2010;95:251–62.
Watzman HM, Kurth CD, Montenegro LM, Rome J, Steven JM, Nicolson SC. Arterial and venous contributions to near-infrared cerebral oximetry. Anesthesiology. 2000;93:947–53.
Reynolds JC, Salcido D, Koller AC, Sundermann ML, Frisch A, Suffoletto BP, Menegazzi JJ. Tissue oximetry by near-infrared spectroscopy in a porcine model of out-of-hospital cardiac arrest and resuscitation. Resuscitation. 2013;84:843–7.
Schön J, Heringlake M, Berger K, Volker Groesdonk H, Sedemund-Adib B, Paarmann H. Relationship between mixed venous oxygen saturation and regional cerebral oxygenation in awake, spontaneously breathing cardiac surgery patients. Minerva Anestesiol. 2011;77:952–8.
Moreno GE, Pilán ML, Manara C, Magliola R, Vassallo JC, Balestrini M, Lenz AM, Krynski M, Althabe M, Landry L. Regional venous oxygen saturation versus mixed venous saturation after paediatric cardiac surgery. Acta Anaesthesiol Scand. 2013;57:373–9.
Zander R, Rehfisch P. Noninvasive measurement of cerebral hemoglobin-oxygen saturation. Anästhesiol Intensivmed Notfallmedizin Schmerzther (AINS). 1997;32(2 Suppl):220–3.
Alboni P, Alboni M, Gianfranchi L. Diving bradycardia: a mechanism of defence against hypoxic damage. J Cardiovasc Med. 2011;12:422–7.
Watkin SL, Spencer SA, Dimmock PW, Wickramasinghe YA, Rolfe P. A comparison of pulse oximetry and near infrared spectroscopy (NIRS) in the detection of hypoxaemia occurring with pauses in nasal airflow in neonates. J Clin Monit Comput. 1999;15:441–7.
Pizza F, Biallas M, Wolf M, Werth E, Bassetti CL. Nocturnal cerebral hemodynamics in snorers and in patients with obstructive sleep apnea: a near-infrared spectroscopy study. Sleep. 2010;33:205–10.
Mohsenin V. Obstructive sleep apnea and hypertension: a critical review. Curr Hypertens Rep. 2014;16:482.
Nishiyasu T, Tsukamoto R, Kawai K, Hayashi K, Koga S, Ichinose M. Relationships between the extent of apnea-induced bradycardia and the vascular response in the arm and leg during dynamic two-legged knee extension exercise. Am J Physiol. 2012;302:H864–71.
Perini R, Tironi A, Gheza A, Butti F, Moia C, Ferretti G. Heart rate and blood pressure time courses during prolonged dry apnoea in breath-hold divers. Eur J Appl Physiol. 2008;104:1–7.
Leuenberger UA, Hardy JC, Herr MD, Gray KS, Sinoway LI. Hypoxia augments apnea-induced peripheral vasoconstriction in humans. J Appl Physiol. 1985;90:1516–22.
Macefield VG, Gandevia SC, Henderson LA. Neural sites involved in the sustained increase in muscle sympathetic nerve activity induced by inspiratory capacity apnea: a fMRI study. J Appl Physiol. 2006;100:266–73.
Heusser K, Dzamonja G, Tank J, Palada I, Valic Z, Bakovic D, Obad A, Ivancev V, Breskovic T, Diedrich A, Joyner MJ, Luft FC, Jordan J, Dujic Z. Cardiovascular regulation during apnea in elite divers. Hypertension. 2009;53:719–24.
Kolb JC, Ainslie PN, Ide K, Poulin MJ. Protocol to measure acute cerebrovascular and ventilatory responses to isocapnic hypoxia in humans. Respir Physiol Neurobiol. 2004;141:191–9.
Wilson MH, Newman S, Imray CH. The cerebral effects of ascent to high altitudes. Lancet Neurol. 2009;8:175–91.
Ainslie PN, Barach A, Murrell C, Hamlin M, Hellemans J, Ogoh S. Alterations in cerebral autoregulation and cerebral blood flow velocity during acute hypoxia: rest and exercise. Am J Physiol Heart Circ Physiol. 2007;292:H976–83.
Rupp T, Leti T, Jubeau M, Millet GY, Bricout VA, Levy P, Wuyam B, Perrey S, Verges S. Tissue deoxygenation kinetics induced by prolonged hypoxic exposure in healthy humans at rest. J Biomed Opt. 2013;18:095002.
Ahn A, Nasir A, Malik H, D’Orazi F, Parnia S. A pilot study examining the role of regional cerebral oxygen saturation monitoring as a marker of return of spontaneous circulation in shockable (VF/VT) and non-shockable (PEA/asystole) causes of cardiac arrest. Resuscitation. 2013;84:1713–6.
Schewe JC, Thudium MO, Kappler J, Steinhagen F, Eichhorn L, Erdfelder F, Heister U, Ellerkmann R. Monitoring of cerebral oxygen saturation during resuscitation in out-of-hospital cardiac arrest: a feasibility study in a physician staffed emergency medical system. Scand J Trauma Resusc Emerg Med. 2014;5:58.
Meex I, De Deyne C, Dens J, Scheyltjens S, Lathouwers K, Boer W, Vundelinckx G, Heylen R, Jans F. Feasibility of absolute cerebral tissue oxygen saturation during cardiopulmonary resuscitation. Crit Care. 2013;17:R36.
Ahn A, Yang J, Inigo-Santiago L, Parnia S. A feasibility study of cerebral oximetry monitoring during the post-resuscitation period in comatose patients following cardiac arrest. Resuscitation. 2014;85:522–6. doi:10.1016/j.resuscitation.2013.
Acknowledgments
Special thanks to all volunteers of the study and to Anja Reckendorf for critical reading of the manuscript. L. Eichhorn was supported by a scholarship of Else-Kröner-Fresenius Stiftung.
Conflict of interest
The authors have no conflicts of interest. The authors have no financial relationship with NONIN Medical’s EQUANOX™. All machines were already available in our University hospital.
Ethical standard
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Author information
Authors and Affiliations
Corresponding author
Additional information
Lars Eichhorn and Felix Erdfelder have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Eichhorn, L., Erdfelder, F., Kessler, F. et al. Evaluation of near-infrared spectroscopy under apnea-dependent hypoxia in humans. J Clin Monit Comput 29, 749–757 (2015). https://doi.org/10.1007/s10877-015-9662-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-015-9662-2