Opinion statement
Management of thrombosis of the dural sinus and cerebral veins (CVT) includes treatment of the underlying condition, antithrombotic treatment, symptomatic treatment, and the prevention or treatment of complications.
Intravenous heparin or subcutaneous low-molecular-weight heparin should be used in acute CVT to prevent thrombus propagation and pulmonary embolism and to increase the chances of recanalization. Anticoagulation is safe and can be used in patients with acute CVT who have intracranial hemorrhagic lesions.
Endovascular thrombolysis (with or without mechanical thrombus disruption) is an experimental treatment to be used in experienced centers for severe cases or patients who fail to improve on anticoagulation. Local thrombolysis is not useful in patients with large infarcts and impending herniation.
In patients with severe headache and papilledema, intracranial hypertension can be reduced and symptoms relieved through a therapeutic lumbar puncture. Hemicraniectomy may be lifesaving in patients with parenchymal lesions leading to herniation.
In patients with acute seizures and supratentorial lesions, antiepileptic drugs should be prescribed. Prophylactic use of these drugs can also be considered for patients with one of these risk factors but should be avoided in patients with neither of them.
To reduce the risk of recurrent deep venous thrombosis of the limbs, vitamin K antagonists are given for a variable period depending on the patient’s inherent risk of thrombosis, aiming at an International Normalized Ratio of 2 to 3.5. If CVT is related to a transient risk factor (eg, pregnancy, infection), we recommend anticoagulants for 3 months. In patients with idiopathic CVT or CVT associated with “mild” thrombophilia, the period of anticoagulation must be extended to 6 to 12 months. In patients with “severe” thrombophilia (eg, two or more prothrombotic abnormalities or antiphospholipid syndrome), anticoagulants should be given for life.
Patients with persistent symptoms of increased intracranial hypertension, visual loss, or both can be treated with repeated lumbar punctures or a lumboperitoneal shunt.
For the prevention of remote seizures, antiepileptic drugs are recommended for patients with seizures in the acute phase and for those who experience a seizure after the acute phase. These drugs can also be considered for patients without seizures who have supratentorial hemorrhagic lesions or motor deficits.
Similar content being viewed by others
References and Recommended Reading
Stam J: Thrombosis of the cerebral veins and sinuses. N Engl J Med 2005, 352:1791–1798.
Bousser MG, Ferro JM: Cerebral venous thrombosis: an update. Lancet Neurol 2007, 6:162–170.
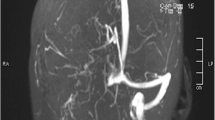
Janjua N: Cerebral angiography and venography for evaluation of cerebral venous thrombosis. J Pak Med Assoc 2006, 56:527–530.
Ferro JM, Canhão P, Bousser MG, et al.; ISCVT Investigators: Early seizures in cerebral vein and dural sinus thrombosis. Risk factors, and role of antiepileptics. Stroke. In press.
Crassard I, Bousser MG: Headache in patients with cerebral venous thrombosis. Rev Neurol 2005, 161:706–708.
deVeber G, Andrew M, Adams C, et al.; the Canadian Pediatric Ischemic Stroke Study Group: Cerebral sinovenous thrombosis in children. N Engl J Med 2001, 345:417–423.
Ferro JM, Canhão P, Bousser MG, et al.; ISCVT Investigators: Cerebral vein and dural sinus thrombosis in elderly patients. Stroke 2005, 36:1927–1932.
Ferro JM, Lopes MG, Rosas MJ Fontes J; VENOPORT Investigators: Delay in hospital admission of patients with cerebral vein and dural sinus thrombosis, Cerebrovasc Dis 2005, 19:152–156.
Kurosu A, Suzukawa K, Amo M, et al.: Perimesencephalic non-aneurysmal subarachnoid hemorrhage caused by cavernous sinus thrombosis: case report. Neurol Med Chir 2007, 47:258–260.
Shukla R, Vinod P, Prakash S, et al.: Subarachnoid haemorrhage as a presentation of cerebral venous sinus thrombosis. J Assoc Physicians India 2006, 54:42–44.
Sigari F, Blair E, Redleaf M: Headache with unilateral pulsatile tinnitus in woman can signal dural sinus thrombosis. Ann Otol Rhinol Laryngol 2006, 115:686–689.
Ferro JM, Canhão P, Stam J, et al.; ISCVT Investigators: Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke 2004, 35:664–670.
Niyasom S, Sithinamsuwan P, Udommongkol C, Suwantamee J: Dural sinus thrombosis in mellioidosis: the first case report. J Med Assoc Thai 2006, 89:242–247.
Edris F, Kerner CM, Feyles V, et al.: Successful management of an extensive intracranial sinus thrombosis in a patient undergoing IVF: case report and review of literature. Fertil Steril 2007, 88:705.e9–705.e14.
Horga A, Santamarina E, Quilez A, et al.: Cerebral venous thrombosis associated with repeated use of emergency contraception [letter]. Eur J Neurol 2007, 14(4):e–5.
Thorat JD, Ng I: Acute dural sinus thrombosis following ingestion of an herbal tonic: case report. J Stroke 2007, 16:232–235.
Papin F, Clarot F, Vicomte C, et al.: Lethal paradoxical cerebral vein thrombosis due to suspicious anticoagulant rodenticide intoxication with chlorophacinone [review]. Forensic Sci Int 2007, 166:85–90.
Balci K, Utku U, Asil T, Büyükkoyuncu N: Deep cerebral vein thrombosis associated with iron deficiency anaemia in adults. J Clin Neurosci 2007, 14:181–184.
Cantu C, Alonso E, Jara A, et al.: Hyperhomocysteinemia, low folate and vitamin B12 concentrations, and methylene tetrahydrofolate reductase mutation in cerebral venous thrombosis. Stroke 2004, 35:1790–1794.
De Stefano V, Fiorini A, Rossi E, et al.: Incidence of JAK2 V617F mutation among patients with splanchnic or cerebral venous thrombosis and without overt chronic myeloproliferative disorders. J Thromb Haemost 2007, 5:708–714.
Colaizzo D, Amitrano L, Iannaccone L, et al.: Gain-offunction gene mutations and venous thromboembolism: distinct roles in different clinical settings. J Med Genet 2007, 44:412–416.
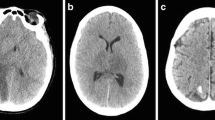
Leach JL, Fortuna RB, Jones BV, Gaskill-Shipley MF: Imaging of cerebral venous thrombosis: current techniques, spectrum of findings and diagnostic pitfalls. Radiographics 2006, 26(Suppl 1):S19–S41.
Ferro JM, Morgado C, Sousa R, Canhão P: Interobserver agreement in the magnetic resonance location of cerebral vein and dural sinus thrombosis. Eur J Neurol 2007, 14:353–356.
Fellner FA, Fellner C, Aichner FT, Mölzer G: Importance of T2*-weighted gradient-echo MRI for diagnosis of cortical vein thrombosis. Eur J Neurol 2005, 56:235–239.
Idbaih A, Boukobza M, Crassard I, et al.: MRI of clot in cerebral venous thrombosis: high diagnostic value of susceptibility-weighted images. Stroke 2006, 37:991–995.
Leach JL, Strub WM, Gaskill-Shipley MF: Cerebral venous thrombus signal intensity and susceptibility effect on gradient recalled-echo MR imaging. AJNR Am J Neuroradiol 2007, 28:940–945.
Rodallec MH, Krainik A, Feydy A, et al.: Cerebral venous thrombosis and multidetector CT angiography: tips and tricks. Radiographics 2006, 26(Suppl 1):S5–S18.
Linn J, Ertl-Wagner B, Seelos KC, et al.: Diagnostic value of multidetector-row CT angiography in the evaluation of thrombosis in the cerebral venous sinuses. AJNR Am J Neuroradiol 2007, 28:946–952.
Girot M, Ferro JM, Canhão P, et al.: ISCVT Investigators: Predictors of outcome in patients with cerebral venous thrombosis and intracerebral hemorrhage. Stroke 2007, 38:337–342.
Canhão P, Ferro JM, Lindgren AG, et al.: ISCVT Investigators: Causes and predictors of death in cerebral venous thrombosis. Stroke 2005, 36:1720–1725.
Del Sette M, Dinia L, Gandolfo C: Brain-to-brain paradoxical embolism through patent foramen ovale after cerebral vein thrombosis. Eur Neurol 2007, 57:176–177.
Favrole P, Guichard JP, Crassard I, et al.: Diffusionweighted imaging of intravascular clots in cerebral venous thrombosis. Stroke 2004, 35:99–103.
Preter M, Tzourio CH, Ameri A, Bousser MG: Long term prognosis in cerebral vein thrombosis: a follow up of 77 patients. Stroke 1996, 27:243–246.
Srinivasan K: Cerebral venous and arterial thrombosis in pregnancy and puerperium: a study of 135 patients. Angiology 1983, 34:731–746
Lamy C, Hamon JB, Coste J, Mas JL: Ischemic stroke in young women: risk of recurrence during subsequent pregnancies. French Study Group on Stroke in Pregnancy. Neurology 2000, 55:269–274.
Merhraein S, Ortwein H, Busch M, et al.: Risk of recurrence of cerebral venous and sinus thrombosis during subsequent pregnancy and puerperium. J Neurol Neurosurg Psychiatry 2003, 74:814–816.
Einhäupl KM, Villringer A, Meister W, et al.: Heparin treatment in sinus venous thrombosis. Lancet 1991, 338:597–600.
de Bruijn SF, Stam J: Randomized, placebo-controlled trial of anticoagulant treatment with low-molecular-weight heparin for cerebral sinus thrombosis. Stroke 1999, 30:484–488.
Nagaraja D, Rao B, Taly AB, Subhash MN: Randomized controlled trial of heparin in puerperal cerebral venous/sinus thrombosis. Nimhans Journal 1995, 13:111–115.
Stam J, de Bruijn SF, deVeber G: Anticoagulation for cerebral sinus thrombosis. Cochrane Database Syst Rev 2002, CD002005.
Lee YH, Lee JY, Kim YS, et al.: Successful anticoagulation for bilateral central retinal vein occlusions accompanied by cerebral venous thrombosis. Arch Neurol 2006, 63:1648–1651.
deVeber G, Chan A, Monagle P, et al.: Anticoagulation therapy in pediatric patients with sinovenous thrombosis: a cohort study. Arch Neurol 1998, 55:1533–1537.
Canhão P, Falcão F, Ferro JM: Thrombolytics for cerebral sinus thrombosis: a systematic review. Cerebrovasc Dis 2003, 15:159–166.
Kirsch J, Rasmussen PA, Masaryk TJ, et al.: Adjunctive rheolytic thrombectomy for central venous sinus: technical case report. Neurosurgery 2007, 60:e577–e578.
Stam J, Majoie BLM, van Delden OM, et al.: Endovascular thrombectomy and thrombolysis for severe cerebral sinus thrombosis. Stroke. In press.
Gosk-Bierska I, Wysokinski W, Brown RD Jr, et al.: Cerebral venous sinus thrombosis: Incidence of venous thrombosis recurrence and survival. Neurology 2006, 67:814–819.
Kenet G, Kirkham F, Niederstadt T, et al.; European Thromboses Study Group: Risk factors for recurrent venous thromboembolism in the European collaborative paediatric database on cerebral venous thrombosis: a multicentre cohort study. Lancet Neurol 2007, 6:595–603.
Einhäupl K, Bousser MG, de Bruijn SF, et al.: EFNS guideline on the treatment of cerebral venous and sinus thrombosis. Eur J Neurol 2006, 13:553–559.
Jilma B, Kamath S, Lip GY: Antithrombotic therapy in special circumstances. I-pregnancy and cancer [review]. BMJ 2003, 326:37–40.
Canhão P, Cortesão A, Cabral M, et al., for the ISCVT Investigators: Are steroids useful to treat cerebral venous thrombosis? Stroke. In press.
Stefini R, Latronico N, Cornali C, et al.: Emergent decompressive craniectomy in patients with fixed dilated pupils due to cerebral venous and dural sinus thrombosis: report of three cases. Neurosurgery 1999, 45:626–629.
Keller E, Pangalu A, Fandino J, et al.: Decompressive craniectomy in severe cerebral venous and dural sinus thrombosis. Acta Neurochir 2005, 94(Supp):177–183.
Vahedi K, Hofmeijer J, Juettler E, et al.; DECIMAL, DESTINY, and HAMLET investigators: Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomised controlled trials. Lancet Neurol 2007, 6:215–222.
Marson AG, Al-Kharusi AM, Alwaidh M, et al.; SANAD Study Group: The SANAD study of effectiveness of valproate, lamotrigine, or topiramate for generalised and unclassifiable epilepsy: an unblinded randomised controlled trial. Lancet 2007, 369:1016–1026.
Marson AG, Al-Kharusi AM, Alwaidh M, et al.; SANAD Study Group: The SANAD study of effectiveness of carbamazepine, gabapentin, lamotrigine, oxcarbazepine, or topiramate for treatment of partial epilepsy: an unblinded randomised controlled trial. Lancet 2007, 369:1000–1015.
National Institute for Clinical Excellence: The epilepsies: the diagnosis and management of the epilepsies in adults and children in primary and secondary care. Clinical Guideline 20, 2004. Available at www.nice.org.uk/CG020NICEguideline. Accessed November 19, 2007.
Bleck TP: Refractory status epilepticus. Curr Opin Crit Care 2005, 11:117–120.
Treiman DM, Walker MC: Treatment of seizure emergencies: convulsive and non-convulsive status epilepticus. Epilepsy Res 2006, 68(Suppl 1):S77–S82.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ferro, J.M., Canhão, P. Acute treatment of cerebral venous and dural sinus thrombosis. Curr Treat Options Neurol 10, 126–137 (2008). https://doi.org/10.1007/s11940-008-0014-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11940-008-0014-0