Case of the Week Archive
Section Editors: Matylda Machnowska1 and Anvita Pauranik2
1University of Toronto, Toronto, Ontario, Canada
2University of British Columbia, Vancouver, British Columbia, Canada
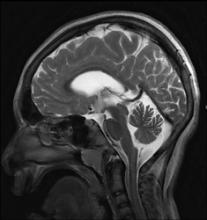
A 13-year-old girl presents with developmental delay from birth, seizures since 6 months of age, and progressive gait disturbances. On examination she demonstrates spasticity in all 4 limbs (lower limbs > upper limbs), microcephaly, and low intelligence quotient.
A 26-year-old man presents at a Level 1 trauma center after being hit by a vehicle traveling at 30 mph (48 km/h). Initial Glasgow Coma Score (GCS) score was 14 and trauma CT survey showed only mild intra-abdominal injuries with lower extremity radiographs showing comminuted, distracted fractures of the right tibia and fibula. Following emergent internal fixation of the right lower leg injuries, the patient developed seizures and a decline in neurologic function (GCS of 3) prompting further neuroimaging.
A 35-year-old, type 2 diabetic woman presents with subacute onset swelling within right nasofacial groove, pain, and fever.
A 13-year-old boy presents with normal birth and developmental history, mild language delay, a 7-year history of complex febrile seizures, and gradually progressive bilateral lower limb weakness.
A 73-year-old man with an unremarkable past medical history presents with diplopia for more than 6 months.
A 29-year-old woman with a history of vague abdominal pain, amenorrhea, and lumbar pain for 3 months is admitted to the hospital because she developed headache and a generalized tonic-clonic seizure.