Abstract
Summary: We report a case of malignant ectopic thymoma in the neck. Contrast-enhanced CT of the neck showed a well-defined inhomogeneously enhancing mass in the left jugulodigastric chain. One year after surgery, the mass had metastasized to the tongue base, and CT of the neck showed an ill-defined densely enhancing mass with lymphadenopathy.
The thymus anatomically originates from the superior neck during early fetal life and descends to the mediastinum. During this descent, remnants of thymic tissue occasionally are implanted along the cervical pathway and may appear later as an ectopic cervical thymus (1). Although rare, malignant thymoma may develop from an ectopic thymus (2). We present a case of malignant thymoma occurring in the left parapharyngeal space of the neck, with metastasis to the tongue base 1 year after surgery.
Case Report
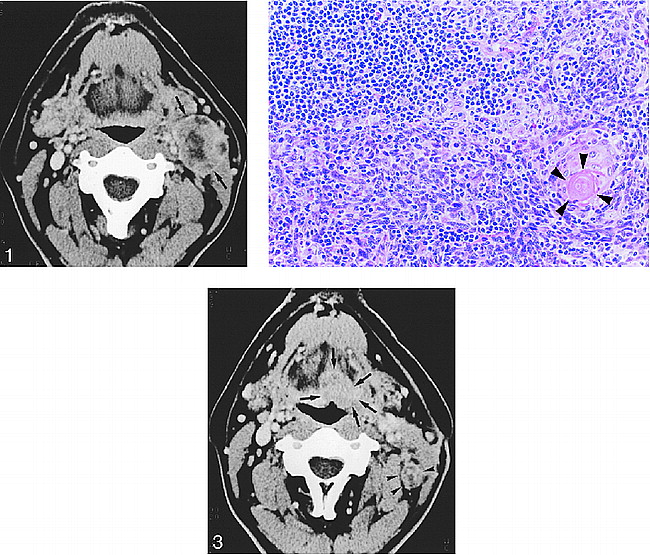
A 65-year-old man presented with a 9-month history of a palpable submandibular mass in the left jugulodigastric area. A physical examination revealed that the mass was 3 cm in diameter, movable, and non-tender. CT of the neck performed at admission showed an approximately 3 × 4 × 4-cm, well-defined mass in the left jugulodigastric chain (Fig 1A). It arose from the level of the pyriform sinus and extended superiorly to the level of the mandibular angle. The mass compressed both the internal carotid artery and the internal jugular vein medially and displaced the common carotid artery anterolaterally. It showed peripheral contrast enhancement with a hypoattenuated center. Several lymph nodes that were smaller than 1 cm were noted in the left posterior neck. Total excision of the tumor was performed. A pathologic examination revealed that the tumor was enclosed by a thick fibrous capsule and composed of a mixture, in varying proportions, of epithelial cells and lymphocytes. Typical Hassall's corpuscles were noted, but there was no evidence of a mitotic figure or cellular atypism. Evidence of any lymph node components was not found in the mass. Pathologic diagnosis was consistent with primary thymoma (Fig 1B). The lymph nodes resected during surgery revealed reactive hyperplasia without tumor cells. One month after surgery, the results of CT of the chest, which was performed to search for a primary site in the chest, were normal.
Contrast-enhanced CT scan of the neck shows a well-defined, round mass in the left jugulodigastric area (arrows). The mass enhances peripherally with central hypoattenuation. It compresses the internal carotid artery medially. Two lymph nodes of less than 1 cm in diameter were also noted in the posterior neck. No evidence of abnormality was seen in left tongue base.fig 2. The tumor is composed of a mixture, in varying proportions, of epithelial cells and lymphocytes. Hassall's corpuscle, which is typically demonstrated in thymoma, is noted (arrowheads) (magnification, ×40).fig 3. Follow-up contrast-enhanced CT scan of the neck, obtained 1 year after surgery, shows a 2 × 3-cm, ill-defined mass in the left tongue base (arrows). This mass is isodense to the tongue muscle. Several conglomerate nodules are noted in left posterior neck (arrowheads), which show central hypoattenuation with peripheral rim enhancement
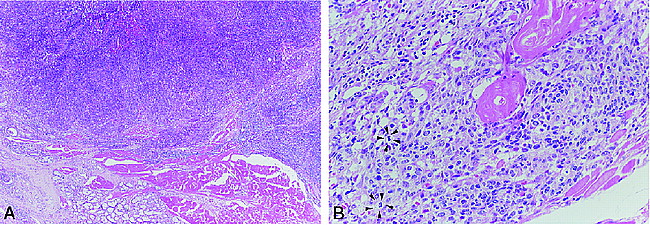
A, Low magnification view of the tongue mass (×40) shows ill-defined infiltrative solid tumor. Tongue tissue, including muscle and salivary gland, is noted inferiorly.
B, High-magnification view of the tongue mass (×200) shows epithelial cells and Hassall's corpuscles. The tumor is more aggressive than primary neck mass and shows some mitosis (arrowheads).
One year after surgery, three nodules were palpated in the posterior neck. A physical examination revealed a 3-cm, exophytic reddish mass in the left tongue base. Contrast-enhanced CT of the neck showed an ill-defined, 2 × 3-cm, densely enhancing mass in the left tongue base (Fig 1C). Multiple, round, conglomerate lymph nodes with central hypoattenuation and a peripherally enhancing rim were noted in the left posterior neck. Biopsy and subsequent surgery, including hemiglossectomy and radical neck dissection, revealed metastatic malignant thymoma (Fig 1D–E). After surgery, radiation therapy was administered.
Discussion
Thymus develops from the ventral portion of the third and fourth pharyngeal pouches. This descends into the anterior mediastinum by the sixth week of gestation. Thymic ectopia results from failure of this migration. Aberrant nodules of thymic tissue are found in approximately 20% of humans. Although the majority of aberrant nodules are located laterally in the neck, ectopic thymic nodules also have been reported in the base of the skull, in the mediastinum, and at the root of the bronchus (1).
Thymic neoplasm arising from an ectopic thymus is rare. To the best of our knowledge, only one case has been reported in the English language literature regarding the imaging findings of the malignant ectopic thymoma (2). In that case, it arose from the posterior mediastinum and had a connecting pedicle between the extrapleural mass and mediastinum. In contrast, the lesion in our case was far from the mediastinum and the results of CT of the chest were normal.
Malignant thymoma is classified into two types: type I, invasive thymoma; and type II, thymic carcinoma (1–3). Type I malignant thymoma (invasive thymoma) behaves in a malignant fashion despite its benign histologic appearance. The distinction between ordinary thymoma and invasive thymoma depends on the demonstration of local invasion or metastasis. Type II malignant thymoma (thymic carcinoma) is comprised of rare tumors of the anterior mediastinum. They are histologically malignant tumors with a clinical course that tends to be much more aggressive than that of type I malignant thymoma. Our case initially was reported to be that of benign thymoma because of the absence of mitosis or infiltration, but 1 year later it was classified as type I malignant thymoma because of metastasis.
The differentiation of benign from malignant thymoma is not always possible. Generally, malignant thymoma of the anterior mediastinum appears as a homogeneous contrast-enhancing mass, with or without local invasion revealed by CT. Occasionally, it has a cystic or necrotic portion (4). Our case showed well-defined, peripheral contrast enhancement with a central low-attenuation area, which was similar to that of the case of mediastinal thymoma (4).
Differential diagnosis in our case included metastatic lymphadenopathy, tumor arising from the tail of the parotid gland, and neurogenic tumor (5). Although the imaging findings are nonspecific, ectopic thymoma should be considered if a patient presents with myasthenia gravis or thymoma-related disease.
Persistence of symptoms in a patient with myasthenia gravis who has undergone a thymectomy has been attributed to thymus remnants. If a patient with myasthenia showed neck mass, as in our case, with or without transitory improvement after thymectomy, ectopic thymoma would be considered (6−8).
We report a case of malignant ectopic thymoma in the neck. Contrast-enhanced CT of the neck showed a well-defined inhomogeneously enhancing mass in the left jugulodigastric chain. The mass metastasized to the tongue base 1 year after surgery, and CT of the neck performed at that time showed an ill-defined densely enhancing mass with lymphadenopathy.
Footnotes
↵1 Address reprint requests to Jung Im Jung, MD, Department of Radiology, St. Mary's Hospital, College of Medicine, The Catholic University of Korea, #62 Youido-dong, Youngdungpo-gu, Seoul 150-010, Korea.
- Received January 6, 1999.
- Copyright © American Society of Neuroradiology