Abstract
Summary: A woman reported painful thrombosis of the superficial femoral artery 16 months after a transfemoral microcatheter was glued into a cerebral arteriovenous malformation and transected at the groin. When the catheter was removed, a portion was found to be incorporated into the wall of the carotid artery. This case demonstrates that portions of a retained microcatheter may be incorporated into the arterial wall while other portions may remain mobile and cause late peripheral arterial symptoms.
Recent technical advances have made embolotherapy an integral part of the management of cerebral AVMs, particularly as an adjunct to surgical ablation or radiotherapy. Embolotherapy is not without risk, and a wide array of technical complications, including carotid dissection, arterial perforation, dissection of feeding vessels, venous and pulmonary embolization, catheter emboli, catheters glued to normal vessels, and retinal artery embolization, have been reported (1). Technical complications have led to temporary or permanent complications, including intracerebral hemorrhage and death, cerebral infarction, subarachnoid hemorrhage with headache, vomiting and seizures, hemiparesis, aphasia, and visual field deficits (1–9).
Relatively few reports of catheters glued into the cerebral circulation have been published (2–7). Debrun et al (1) found that over a 15-year period, 29 microcatheters were inadvertently glued into a feeding artery in 936 superselective glue injections for cerebral AVMs in 233 patients (3.1% of injections; 12.4% of patients). Only two of these patients incurred neurologic deficits in the territory of the retained microcatheter. Another group reported one late neurologic event, but this occurred during a subsequent session of embolotherapy (3). Most reports of glued catheters have occurred using isobutyl-2-cyanoacrylate (IBCA), or n-butyl cyanoacrylate (NBCA), and are secondary to technical mishaps, including overzealous embolization, too rapid polymerization, and excessive reflux of adhesive around the catheter tip (4). Catheter segments left in place are intraarterial foreign bodies and may represent an ongoing risk for thromboembolic complications. The natural history of retained catheter fragments has not been reported.
Case Report
A 27-year-old woman with seizures since childhood was found to have a 4-cm frontal arteriovenous malformation (AVM) supplied by sylvian branches of the right middle cerebral artery. In August 1995, the feeding pedicles were occluded with liquid tissue adhesive using a Balt 1.8F flow-directed microcatheter via the right common femoral artery. The catheter was inadvertently glued into the AVM, and could not be removed. The catheter was transected at the groin, and allowed to retract into the common femoral artery. The patient received anticoagulant therapy for 48 hours and was maintained on aspirin. She then had gamma knife radiosurgery with excellent anatomic results.
Sixteen months later, intermittent sharp pains developed in the right side of the groin. The pain progressed to a constant stabbing sensation, which was aggravated by ambulation. Physical examination revealed marked tenderness to palpation in the right side of the groin, but no mass was present. The femoral and pedal pulses were palpable, and ankle-brachial indexes were 1.0. Results of a neurologic examination were normal. Duplex sonography and arteriography showed occlusion of the proximal right superficial femoral artery with the distal tip of the retained catheter visible in the thrombus.
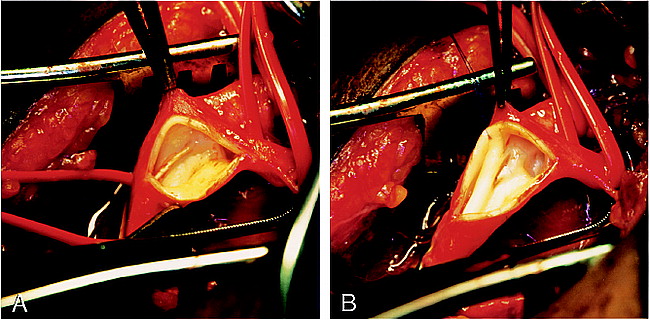
With the use of regional anesthesia and systemic heparin anticoagulation, the carotid bifurcation was exposed, controlled, and opened. The catheter was free in the lumen of the mid–common carotid artery, but became incorporated in fibrous plaque at the carotid bifurcation (Fig 1A). The catheter was embedded as far distally in the internal carotid artery as could be seen (about 3 cm). It was divided in the mid–common carotid artery, and the proximal segment (about 68 cm) was withdrawn. The free end of the catheter was sutured to the arterial wall where it entered the plaque and trimmed flush with the surface (Fig 1B). Postoperatively, the patient reported immediate and complete resolution of her groin pain. She remains neurologically intact with no right leg symptoms 6 months after surgery.
27-year-old woman with retained microcatheter causing intermittent sharp pains in the right side of the groin.
A, Intraoperative photograph of the carotid bifurcation shows the retained microcatheter passing from an intraluminal position into fibrous plaque at the common carotid flow divider.
B, Intraoperative photograph of the carotid bifurcation shows the transected catheter sutured to the arterial wall.
Discussion
Our case illustrates that a retained catheter may behave differently in different areas along its course in the vascular tree. Portions of the catheter in the aorta and the common femoral artery were freely mobile 16 months after placement and were associated with thrombotic occlusion of the superficial femoral artery. In contrast, the segment of the catheter in the carotid was in contact with the arterial wall and became incorporated in fibrous plaque. The extent of incorporation of the catheter in the distal internal carotid or in the middle cerebral artery in our case is not known. To our knowledge, this is the first report to confirm incorporation of a catheter into the arterial wall in humans. It is likely that the catheter became incorporated into the vessel wall only at points of constant contact. A retained catheter may produce local arterial injury, incite an inflammatory or proliferative response, and may be a risk factor for accelerated atherosclerosis. Although duplex sonography did not show significant intraluminal narrowing of the carotid in our case, the long-term behavior of the catheter-associated fibrous lesion is not known.
There have been reports of same-day removal of retained catheters with a snare (1, 5), incidental or intentional removal during surgical excision of an AVM (1, 5), and presumptive incorporation of retained catheters into the internal carotid or middle cerebral artery. In most instances, the retained catheter has simply been transected at the puncture site (4, 6) and allowed to retract into the iliac system. The length of retained catheter in our case is greater than that reported by Debrun et al (1). A shorter length would leave the free proximal end of the catheter in the mid-thoracic or abdominal aorta. This location in a larger-caliber artery that is not subject to exercise-related motion may explain the absence of peripheral symptoms or complications in other reports.
Conclusion
In patients with a retained catheter and peripheral arterial symptoms, surgical removal of the bulk of the catheter is indicated. Our case illustrates that this can be accomplished safely and effectively through a carotid approach. Because intraluminal portions of retained catheters may be sources of future emboli or peripheral arterial complications, long-term antithrombotic therapy is indicated. When retained catheters pass through the cervical carotid system, there is a risk of arterial injury and formation of hypertrophic plaque. Periodic monitoring of the carotid bifurcation with duplex sonography is indicated to assess this possibility.
Footnotes
References
- Received November 20, 1997.
- Accepted after revision April 14, 1998.
- Copyright © American Society of Neuroradiology